Ever feel that uncomfortable bloated feeling after a big meal, or wonder why you’re suddenly more sluggish after lunch? Your gut is trying to tell you something, and the good news is that most of those signals can be soothed with a few simple, science‑backed habits.
Below is a friendly, step‑by‑step playbook that blends the latest research on fiber, probiotics, GI‑tract biomarkers, and inflammation biomarkers with real‑world tricks that gastroenterologists in Reno swear by. No fluff—just clear actions you can start today.
Why Gut Matters
What Is Digestive Health?
Digestive health is the ability of your gastrointestinal (GI) tract to break down food, absorb nutrients, and eliminate waste efficiently. When this system works smoothly, you enjoy steady energy, a stronger immune system, and even a clearer mind.
Whole‑Body Connection
Studies show that an unhealthy gut can fuel metabolic syndrome, raise inflammation biomarkers, and weaken immunity. A leaky gut, for instance, lets tiny particles slip into the bloodstream, sparking chronic inflammation that can worsen blood sugar and cholesterol levels.
Quick Symptom Map
| Common Symptom | Possible Underlying Issue |
|---|---|
| Frequent bloating | Low fiber intake or dysbiosis |
| Heartburn after meals | Acid reflux, stress, high‑fat foods |
| Irregular bowel movements | Dehydration or lack of soluble fiber |
| Sudden fatigue | Malabsorption of nutrients |
| Random weight gain | Metabolic syndrome indicators |
Core Gut Pillars
Fiber Fuel
Soluble vs. Insoluble
Soluble fiber (found in oats, beans, and apples) dissolves in water, forming a gel that feeds friendly bacteria and helps lower cholesterol. Insoluble fiber (whole‑grain breads, nuts, and vegetables) adds bulk to stool, keeping things moving.
Daily Targets & Sample Menu
Aiming for at least 25 grams of fiber a day is a good start. Here’s a quick “fiber‑filled day”:
• Breakfast – oatmeal topped with berries and a sprinkle of chia seeds.
• Lunch – quinoa salad with chickpeas, spinach, and sliced bell peppers.
• Snack – an apple with a handful of almonds.
• Dinner – baked salmon, roasted sweet potatoes, and steamed broccoli.
Want more ideas on balancing your meals? Check out this guide on GI tract health for deeper tips.
Probiotic Power
Food Sources
Probiotic‑rich foods act like a friendly neighborhood watch for your gut. Add these to your plate:
• Yogurt with live cultures (no added sugar).
• Kefir, the tangy fermented milk drink.
• Kimchi or sauerkraut – crunchy, sour, and full of lactobacilli.
• Miso and tempeh for a plant‑based probiotic punch.
When Supplements Help
If you’re on antibiotics or travel often, a high‑quality probiotic supplement can fill the gap. Look for strains like Lactobacillus rhamnosus and Bifidobacterium longum, which have the most research backing for IBS relief.
Curious about how these tiny allies are measured? Learn about GI tract biomarkers to see what your doctor might test.
Hydration & Enzymes
Water Intake
About 1.2 liters (6‑8 cups) of water daily keeps stool soft and helps fiber do its job. If you’re upping fiber, sip even more to avoid constipation.
Natural Enzyme Boosters
Foods like pineapple (rich in bromelain) and papaya (papain) contain digestive enzymes that break down proteins and fats, easing bloating after a heavy meal.
Move, Sleep, & Stress
Exercise Benefits
Even a brisk 20‑minute walk, four times a week, can improve bowel motility. A 2014 HealthySD study found that regular walking reduced bloating and increased regularity for most participants.
Sleep Hygiene
Aiming for 7‑9 hours of quality sleep helps regulate hormones that control hunger and gut motility. Keep the bedroom dark, screen‑free, and cool for the best rest.
Stress Management
Stress spikes cortisol, which can increase stomach acid and slow digestion. Try a 5‑minute deep‑breathing routine before meals, or a short yoga flow after work. You’ll notice less heartburn and a calmer gut.
When to See a Doctor
Red‑Flag Symptoms
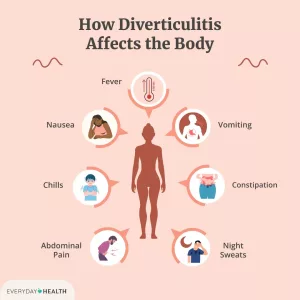
If you experience any of these, schedule a visit with a gastroenterologist promptly:
- Persistent abdominal pain or severe cramping.
- Unexplained weight loss.
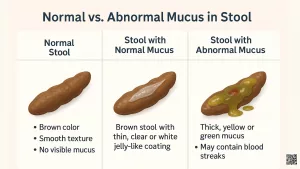
- Blood in stool or black/tarry stools.
- Vomiting that won’t stop.
- Symptoms that last more than four weeks despite lifestyle changes.
Biomarker Testing
Doctors may order stool tests for calprotectin, fecal occult blood, or a comprehensive gut microbiome panel. These inflammation biomarkers can reveal hidden gut inflammation even when you feel okay.
Biomarker Boost
What Are GI‑Tract Biomarkers?
Biomarkers are measurable substances that give clues about how your gut is functioning. Common ones include:
- Calprotectin – signals intestinal inflammation.
- Fecal Immunochemical Test (FIT) – screens for hidden blood.
- Short‑Chain Fatty Acids (SCFAs) – byproducts of fiber fermentation that support colon cells.
Link to Metabolic Health
Elevated inflammatory markers in the gut often mirror the same rise in metabolic syndrome indicators like fasting glucose and waist circumference. In other words, caring for your gut can be a shortcut to keeping your heart and metabolism in check.
Case Snapshot
Take “Anna,” a 42‑year‑old graphic designer who struggled with occasional IBS. After a simple stool test showed high calprotectin, her doctor suggested a targeted probiotic, a fiber‑boosting diet, and regular low‑impact exercise. Within three months, her IBS severity score dropped by 45 % and her energy levels rebounded.
Tools & Resources
Daily Checklist
Print this quick checklist and keep it on your fridge:
- ☑ Add two high‑fiber foods to each meal.
- ☑ Enjoy one probiotic‑rich snack daily.
- ☑ Drink a glass of water every two hours.
- ☑ Take a 20‑minute walk after dinner.
- ☑ Practice a five‑minute breathing exercise before bed.
Helpful Apps
Apps like MyFitnessPal (for tracking fiber) and Headspace (for guided stress relief) make it easy to stay consistent.
Local Support in Reno
If you need a professional opinion, the Digestive Health Center offers board‑certified gastroenterologists who can interpret biomarker results and tailor a plan just for you. Their friendly staff makes the appointment process painless.
Your 7‑Day Action Plan
Ready to put knowledge into motion? Follow this simple week‑long roadmap.
Day 1 – Fiber Focus
Kick off with a bowl of oatmeal topped with blueberries and a tablespoon of ground flaxseed. Aim for 10 g of fiber at breakfast alone.
Day 2 – Probiotic Boost
Swap your usual coffee creamer for a splash of kefir in a smoothie. Add a banana and a handful of spinach for extra micronutrients.
Day 3 – Hydration Sprint
Carry a reusable water bottle and set a reminder to sip every 30 minutes. If plain water feels boring, infuse it with cucumber slices or mint.
Day 4 – Move More
Take a 20‑minute brisk walk after dinner. Notice how your stomach feels afterward—many people report reduced bloating.
Day 5 – Stress Reset
Before bedtime, try a 5‑minute box‑breathing exercise: inhale for 4 seconds, hold for 4, exhale for 4, hold for 4, repeat.
Day 6 – Enzyme Aid
Enjoy a fresh pineapple slice after lunch. The natural bromelain helps break down protein and can ease post‑meal heaviness.
Day 7 – Review & Reflect
Check off your daily checklist, note any changes in energy, digestion, or mood, and decide which habits you’ll keep. If symptoms persist, consider booking a consult to explore biomarker testing.
Conclusion
Good digestive health isn’t a mysterious secret—it’s the result of everyday choices that support your gut’s natural balance. By loading up on fiber, welcoming friendly bacteria, staying hydrated, moving regularly, and managing stress, you give your GI tract the tools it needs to work efficiently and keep inflammation at bay.
Use the quick‑checklist and 7‑day plan above, monitor how you feel, and don’t hesitate to reach out to a qualified gastroenterologist if any red‑flag symptoms linger. Your gut will thank you with smoother digestion, steadier energy, and a stronger immune system.






















Leave a Reply
You must be logged in to post a comment.