What are GI‑tract biomarkers? In plain English, they’re tiny clues—molecules you can find in stool, blood, breath or tissue—that tell you how your stomach, intestines and colon are doing. Think of them as the body’s status updates for the digestive system.
Why should you care? Because these markers can spot inflammation, flag metabolic‑syndrome risk, point to early‑stage cancer, and even guide the success of a new diet—often before you feel any symptoms. In short, they give you a head start on keeping your gut happy and your whole body thriving.
What Are GI Biomarkers
Definition and basic science
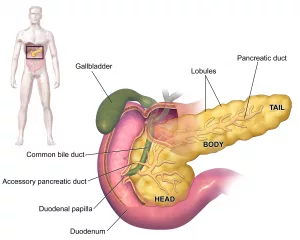
GI‑tract biomarkers are measurable substances—proteins, DNA fragments, metabolites, gases—that reflect the health or disease state of the gastrointestinal (GI) lining. They arise from three main sources:
- Microbial metabolites (short‑chain fatty acids, bile acids, tryptophan derivatives)
- Host proteins (calprotectin, lactoferrin, zonulin)
- Genetic material (circulating tumor DNA, stool‑based DNA panels)
How they are collected
Collecting a biomarker is usually a lot less invasive than an endoscopy. You can provide a sample of stool at home, give a quick blood draw, blow into a breath kit, or, in a clinical setting, hand over a tiny mucosal swab. Each matrix has its own pros and cons—stool is great for microbiome signals, blood captures systemic inflammation, breath picks up gas‑producing bacteria, and biopsies give the most detailed picture but are, well, more involved.
Main Types & Meaning
| Biomarker | Sample | What It Indicates | Typical Use |
|---|---|---|---|
| Fecal calprotectin / lactoferrin | Stool | Intestinal inflammation | Differentiate IBD vs. IBS (fecal lactoferrin study) |
| Short‑chain fatty acids (SCFAs) | Stool | Microbial health, barrier integrity | Diet‑based monitoring |
| Glucagon‑like peptide‑2 (GLP‑2) | Blood | Mucosal repair, nutrient absorption | Post‑surgical recovery |
| Fecal occult blood & DNA panels | Stool | Early colorectal cancer | Screening programs |
| Breath hydrogen & methane | Breath | Small‑intestine bacterial overgrowth (SIBO) | Functional GI complaints |
| Serum zonulin | Blood | Tight‑junction permeability (“leaky gut”) | Metabolic‑syndrome risk |
| Metabolomic panels (bile acids, tryptophan metabolites) | Blood/Urine | Cancer‑linked metabolic shifts | Machine‑learning early detection (novel biomarkers of gastrointestinal cancer) |
Inflammation biomarkers
Calprotectin and lactoferrin are the dynamic duo of gut inflammation. When neutrophils rush to the intestinal lining, they dump these proteins into the stool. Levels above 250 µg/g (calprotectin) or 15 µg/g (lactoferrin) usually scream “active inflammation” and push doctors toward an endoscopic work‑up. For a deeper dive, see the clinical application of fecal biomarkers review.
Metabolic‑syndrome indicators
Ever heard of “leaky gut”? Serum zonulin is the gatekeeper that tells us whether the intestinal barrier is too porous. High zonulin often pairs with altered SCFA ratios and predicts insulin resistance, a core component of metabolic syndrome indicators. In practice, tracking these markers can add a gut‑centric layer to your cardio‑vascular risk score.
Cancer‑related biomarkers
Early detection is the holy grail of oncology. Recent machine‑learning models have identified signatures made up of specific gut bacteria and metabolites that flag gastric or colorectal cancer months before imaging does. While still emerging, these panels hold promise for a future where a simple stool test could trigger life‑saving surveillance.
Clinical Applications
Early detection of GI cancers
Imagine getting a heads‑up that a tumor might be forming, simply because a handful of microbes have shifted. A 2021 study demonstrated that a composite of bacterial taxa and bile‑acid profiles predicted gastric cancer with over 85 % accuracy (novel biomarkers of gastrointestinal cancer). For patients at high risk, such a test could be the difference between a curable early intervention and a late‑stage battle.
Managing inflammatory bowel disease (IBD)
If you’ve ever felt the dread of an IBS vs. IBD misdiagnosis, you’ll appreciate how fecal calprotectin turns the tide. A rising level after a flare can alert your gastroenterologist that the disease is active, prompting a medication tweak before you even feel the next cramp. Conversely, a low level often spares you an unnecessary colonoscopy.
Guiding dietary and lifestyle changes
SCFAs like butyrate are the fuel for colon cells. Low butyrate often points to a low‑fiber diet or a disrupted microbiome. By measuring SCFA concentrations, clinicians can prescribe specific pre‑biotic fibers or probiotic strains, tailoring nutrition to the chemistry of your gut. It’s like a personalized recipe for gut happiness.
Risk stratification for metabolic syndrome
When zonulin climbs, it’s a red flag that the gut barrier may be letting inflammatory molecules into the bloodstream—a pathway linked to obesity, type‑2 diabetes, and heart disease. Pairing zonulin with fasting insulin and lipid panels creates a more nuanced picture of your metabolic health, helping you and your doctor decide when to intensify lifestyle interventions.
Practical workflow for primary‑care
Here’s a quick algorithm you might see on a clinic’s wall:
- Patient reports chronic abdominal pain or irregular stools.
- Order fecal calprotectin (or lactoferrin) as the first screen.
- If elevated, refer for colonoscopy; if normal, consider breath test for SIBO or dietary review.
- For patients with risk factors (family history of cancer, metabolic syndrome), add a stool DNA panel or zonulin test.
Benefits & Risks
Benefits
These tests are generally non‑invasive, cheap compared with imaging, and can catch disease early—giving you a better chance at successful treatment. They also empower you to monitor progress at home, turning you into an active participant in your health journey.
Risks & limitations
No test is perfect. Diet, medications, and even the time of day can sway results. A false‑positive may cause anxiety and unnecessary procedures; a false‑negative might lull you into a false sense of safety. That’s why biomarkers should always be interpreted in the context of symptoms, physical exam, and, when needed, confirmatory diagnostics.
Balancing act
Think of biomarkers like weather forecasts. A sunny forecast doesn’t guarantee sunshine, but it helps you decide whether to bring an umbrella. Likewise, a high calprotectin level isn’t a definitive diagnosis of IBD, but it tells you that a deeper look is warranted.
Testing & Interpretation
Preparing the patient & sample collection
For stool tests, most labs provide a kit with a small collection device and detailed instructions—no gymnastics required. Blood draws are usually done fasting, especially if you’re checking zonulin or metabolomic panels. Breath tests ask you to fast overnight and avoid certain foods the day before.
Laboratory methods
Most protein biomarkers (calprotectin, lactoferrin) use ELISA kits—simple lab plates that glow when the target protein is present. DNA‑based stool tests rely on PCR amplification, while metabolomic panels use mass spectrometry to quantitate dozens of tiny molecules at once. Each method has a trade‑off between cost, speed, and depth of information.
Reading the report
Typical reports show the result, a reference range, and an interpretive comment. For example, “Calprotectin = 312 µg/g (Reference < 50 µg/g): indicates active intestinal inflammation." If a result falls into a "borderline" zone, clinicians often repeat the test in 4–6 weeks to see if the trend is upward or downward.
Integrating results into care plans
Here’s a template you might hear from a doctor:
If calprotectin > 250 µg/g → repeat in 4 weeks.If still high → schedule colonoscopy.If < 50 µg/g → consider functional IBS work‑up, lifestyle changes.
Such clear thresholds keep both patients and providers on the same page, reducing confusion and unnecessary visits.
Expert Insights & Credibility
Professional voice
Dr. Anthony Hobson, a leading gastroenterologist, recently emphasized at a webinar that "breath biomarkers are the future of non‑invasive GI screening," especially for detecting early bacterial overgrowth and even gastric cancer. His optimism mirrors the growing body of research that backs up these claims.
Real‑world story
Meet Maya, a 38‑year‑old teacher who spent years battling vague abdominal cramping. Traditional blood work was normal, and doctors chalked it up to stress. After a single stool calprotectin test spiked at 480 µg/g, she was referred for endoscopy, which revealed early‑stage Crohn's disease. A timely diagnosis meant she started treatment before complications set in, and today she's back to teaching full‑time with her favorite yoga class on the weekends.
Trusted sources
Our recommendations draw on peer‑reviewed journals such as World Journal of Gastrointestinal Pharmacology & Therapeutics, the open‑access article on fecal biomarkers (clinical application of fecal biomarkers), and the cutting‑edge metabolomics research (novel biomarkers of gastrointestinal cancer). By grounding the discussion in reputable science, we aim to give you information you can truly trust.
Putting It All Together
So, why should GI tract biomarkers matter to you? Because they turn invisible gut activity into readable data, letting you and your healthcare team act before symptoms take over. They're not magic bullets—no single number can replace a thoughtful conversation with your doctor—but they are powerful tools in the toolbox of modern GI tract health management.
Whether you're curious about your gut's microbiome, worried about a family history of colorectal cancer, or simply want to know why a new supplement makes you feel better, understanding biomarkers empowers you to ask better questions and make smarter choices.
Take the Next Step
If any of the markers above sparked your interest, consider talking to your primary‑care provider about a baseline stool calprotectin or a simple blood panel for zonulin. Ask how you might incorporate a breath test for SIBO if you often feel bloated after meals. And remember, a healthy gut is a lifelong ally—nurture it with fiber, stay hydrated, manage stress, and keep an eye on those biomarkers as your personal health dashboard.
What will you explore first? Share your thoughts, and let's keep the conversation going. Together we can bring the science of GI tract biomarkers out of the lab and into everyday living—because a well‑informed gut is a happy gut.






















Leave a Reply
You must be logged in to post a comment.