“At first, I thought it was nothing…” You ever have that feeling? One minute, you’re sipping coffee like normal. The next, your world starts spinning, your ear feels plugged, and you’re wondering if sleep deprivation is finally catching up to you. Yeah, I’ve been there. You brush it off, right? Maybe chalk it up to stress, or that one time you rode a rollercoaster and felt weird afterward. But then it happens again. And again. Suddenly, you’re Googling words like Ménière disease diagnosis at 2 a.m., feeling like you’re trapped in a game of spot-the-difference between your symptoms and a medical mystery.
Let’s talk about it—like friends. Because if you’re here, you’re probably stuck in that same loop of confusion, frustration, and a whole lot of “why does this keep happening to me?” And here’s the kicker: Ménière’s is frustratingly hard to nail down, even for doctors.
Frustrating Diagnosis?
You’re not imagining things, and you’re definitely not alone. Ménière disease diagnosis is like trying to solve a puzzle with missing pieces. See, there’s no blood test, no quick scan to point and go “aha!” It’s all about symptom tracking, ruling stuff out, and hoping your doc really listens. But what if things aren’t that simple?
Why Ménière’s Feels Like a Wild Goose Chase
Dizzy spells? Check. Muffled hearing in one ear? Check. Ringing in your ears that won’t quit? Double check. But here’s the catch: those same symptoms show up in other vestibular disorders, like vestibular migraine diagnosis or benign paroxysmal positional vertigo (BPPV). And you know what that means—slower answers, more waiting, and way too many appointments.
Imagine your doctor scribbling notes during your first visit and saying, “Hmm, we’ll need to watch this.” Then comes weeks of balance tests—like electronystagmography (fancy eye-movement tracking), rotary-chair testing (not a rollercoaster, but still destabilizing), and electrocochleography (checking the inner ear’s response to sound waves)—all to basically eliminate other suspects. Tot up your symptoms, cross-reference test results, and bam: if everything else is ruled out, they might finally whisper, “It could be Ménière’s.”
How Long Does This Take? “Hold Your Horses…”
The average time until diagnosis? Hold your horses… A shocking 2–5 years [1]. Yep, 20% of folks wait over five years just to get a name for their symptoms. That’s not just inconvenient; it’s real messy for your mental health and relationships. You’re living with a daily side of “What if something else is wrong?”
I remember talking to a friend (let’s call him Dave) who was misdiagnosed with migraines for two years. By the time they figured it was Ménière’s, his hearing had dropped in one ear for good. It took longer than it should have. Just saying this isn’t a fast lane, but we’ll get through it together, promise.
Table: Classic Triggers vs. Ménière Red Flags
| Condition | Classic Symptom | Ménière Red Flags |
|---|---|---|
| Vestibular Migraine | Sudden vertigo with headaches | No hearing loss or ear pressure |
| Benign Paroxysmal Positional Vertigo | Vertigo triggered by movement | Quick episodes (under a minute), no tinnitus or hearing loss |
| Ménière’s Disease | Episodes of vertigo, ringing in ears | Hearing loss confirmed, multiple episodes spanning weeks-months |
Ménière vs. Vestibular Migraine: Isn’t It All Just Vertigo?
The line between Ménière disease diagnosis and vestibular migraine diagnosis gets blurrier than your vision during an attack. Both of these conditions can knock you sideways:
- Episodes of room-spinning vertigo
- Ear pressure or tinnitus
- Nausea and fatigue
But here’s the catch: timing and tracking symptoms make all the difference. With Ménière’s, those dizzy spells weren’t just random. You probably noticed them lasting at least 20 minutes—sometimes stretching out like a Taylor Swift concert—while vestibular migraine episodes often come and go as swiftly as a coffee run. Fun fact? Ménière’s attacks come with hearing loss, and VM doesn’t. Oh, we’re just getting warmed up.
Getting It Right: Why It Matters
So I ask you: would you treat heartburn like a heart attack? Probably not. Same goes for these two. If your doctor says “migraine” when it’s Ménière, your management plan just misses the target. Conversely? Sending someone through Ménière’s protocols for VM means unnecessary stress and treatment overload.
Back in 2023, a research team slammed the point hard: correct differentiation equals better outcomes [2]. Imagine starting a diet or treatment plan that doesn’t even match what’s going on inside your head (literally). Feelings of helplessness, fatigue, and accidentally chewing out your family over something trivial? Yep, all real things.
How the Pros Spot the Difference: Inner Ear Experts Engineered This
The golden rule isn’t always obvious: the labyrinth-like complexities of the inner ear need someone who eats, sleeps, and breathes balance disorders. You know what most doctors suck at? Spots like inner ear damage or hearing trends that spiral into something bigger unless caught early.
Hydrops MRI: A Real Glimpse Into The Inner Ear
Now hold up. As of late 2024, there’s a tool that helps tease MD and VM apart—endolymphatic hydrops MRI. Let me explain:
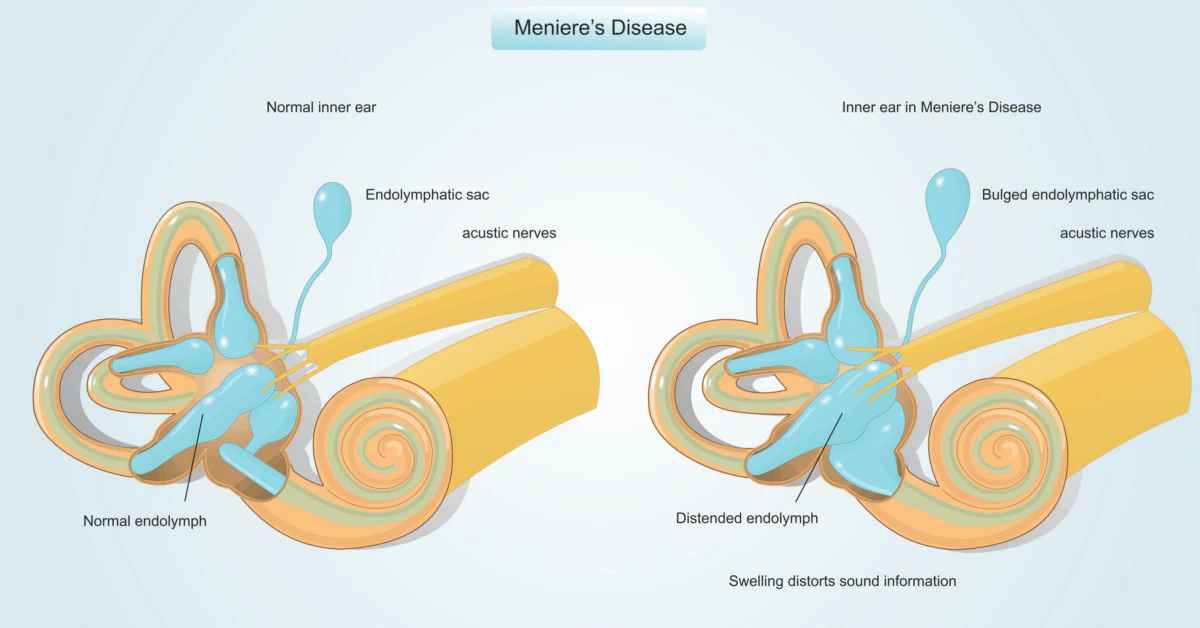
Picture the inner ear. Tiny, delicate fluid-filled sacs. But when those sacs swell with fluid (endolymphatic hydrops), they’re a bit like balloons—problematic and full of unwanted pressure. Hydrops gets named as either cochlear (related to hearing) or vestibular (related to balance). Both sacs dulled with buildup? That’s a classic feature of Ménière’s. VM? It shows less coordination in the inner ear.
So What Can Hydrops MRI Actually Do?
A groundbreaking discovery in 2024 threw the diagnostic strategy a curveball [3]. Using cochlear hydrops MRI and vestibular hydrops MRI, researchers pinpointed patterns unique to Ménière’s. CEH (that’s cochlear endolymphatic hydrops), VEH (you guessed it—vestibular), or both: the imaging reveals them clearly.
Buuut. Before you book your MRI du jour, here’s the gap: accessibility. It’s not some around-the-corner scan you schedule post-brunch. These tests are still a novelty unless you’re near specialized centers and blessed with patient insurance plans. So MRI helps. But, again, folks, we aren’t at perfect resolution yet.
New Frontier, Old Tangles
Even though MRI for Ménière disease got folks excited? This doesn’t mean we’ve solved it perfectly. Some scientists say current criteria are still evolving—who gets tagged as Ménière’s might change in the future. And what about patients already diagnosed? Guh. Could be messy. Could mean revisiting old files and saying, “oh wait.” Still—progress!
From Working Days to Waiting Rooms: The Journey of a Ménière’s Patient
We all know this journey isn’t simple. Shuffling in and out of clinics, jotting symptoms on napkins, obsessively timing dizzy episodes—oh yeah, been there, done that.
1. Tracking Symptoms Like Your Health Hinges on It—Because It Does
If you’re starting this journey, tracking symptoms is your secret weapon. Vertigo lasting more than 20 minutes? Hearing dips over days or weeks? Deaf ear pressure getting stronger? Write each one down like your life depends on it (trust me, it kinda does).
2. On a Vertigo Attack: Managing the Mayhem
Tips for your next dizzy panic attack: find a safe corner. Slow your breathing. Hydrate. Avoid screen scrolling (unless you loved Jeff Goldblum rides through pixelated chaos). And try not to panic when the meds kick in and you feel okay-ish—your body’s trying its best, even if it’s making a mess.
H3: Why Fixing VM vs MD Needs A Clear Plan
Correct identification of the inner issue means no accidentally hopping on VM meds that could let Ménière’s get worse. And no experimental diet relief plans that leave you feeling like you’re choking on sadness and kale. (Yes, when I said “cut salt, caffeine, and alcohol,” it sounded better. Instant difference? Probably not a typo.)
From Past to Present: Medical Milestones You Should Know
Imagine this: 1861. A French doc named Prosper Ménière strolls into a clinic and says, “OMG, it’s not the brain—your ear’s the problem.” And just like that, the first visible shift in ear disease started.
Fast forward to 1956. Hallpike cranks out something called the caloric test—still used today. Pour hot/cold water into your ear, watch the eyes, and guess what, you might get diagnosed faster. In 2020, DIX-Hallpike criteria made its rounds too—detecting all sorts of weird stuff but clarified BPPV vs Ménière’s in the end.
And now? Well, we arrive at 2024 and those chunky endolymphatic hydrops MRI findings. Trust me, if you’d met a 1940s patient hearing this tech existed, they’d ask, “MRI instead of surgery? Count me IN.”
Future Hope: Where’s Ménière’s Diagnosis Going?
You might ask, “Did we just break through something momentous?” The answer’s yes—be kind of a big deal. But can it fix everything? Nope.
Will There Be Reliable Biomarkers?
Hunting for biomarkers is like trying to develop a symptom fingerprint we can prick a finger for. Cool, plausible, but not yet. Genetics studies from the American Hearing Research Foundation found some genes might clue us in [4]. That’s a lot to wrap up in one medical note—but wow, if that pans out, future messengers might get an easy diagnosis instead of your delay drama.
Where Do You Fit While We Wait for a Medical Revolution?
Simple truth: act now but stay flexible. If you suspect MD, drowning deeper than ever, line up appointments with ENT specialists or neurologists who’ve seen cases like yours. If dietary changes soothe you, yeah stick with that—but ask your doc if exclusive fixes suit your needs. And keep those symptoms under daily watch. Your story really matters because it builds the case for you, not against it.
Table: Traditional VS Newer Approach to Ménière Diagnosis
| Traditional | Newer (2024) |
|---|---|
| Caloric testing, audiometry | Endolymphatic hydrops MRI, stating where fluid’s built up |
| Ruling out—the go-to method | DIrect signs of hydrops separate MD from VM |
| Testing over time | Screening time potentially cut down |
Wrap All of This Up?
The long goodbye to routine life with Ménière’s diagnosis is tough. Symptoms overlap like Legos taken from your kid mid-building; treatment is evolving but still far from user-friendly. BUT! Hydrops MRI isn’t just buzz. We’ve got wind in our sails, moving toward more answers than guesswork.
Love the hurdles? Nope. But do we have something to work with? Absolutely. Track, adapt, lean on specialists, and hold fast while science fine-tunes imaging and biomarkers. If you’ve had any of the symptoms—you’ve got my empathy, but more importantly, you’ve got options. The hustle continues until we get your golden hour back.
Catch up soon, yeah? Share your stories. Say hi. What worked—or flopped—on your journey? Drop a line, even if you’re spinning while you type.
Talk to your ENT friends first, stay tuned for breakthroughs, and keep the faith.
References:- [1] PMC on Delayed Diagnoses
- [2] Frontiers in Neurology (2024) on VM vs MD
- [3] Hydrops imaging in MD diagnosis
- [4] Research into genetic links for MD






















Leave a Reply
You must be logged in to post a comment.