Hey there! If you’ve been Googling “Methoxsalen Medicare coverage” you’re probably looking for a clear answer without wading through a mountain of legal‑sounding jargon. Good news – you’re in the right spot. I’m going to walk you through the basics, the nitty‑gritty of Medicare rules, and even share a couple of real‑world stories so you can feel confident navigating this maze. Grab a cup of coffee, settle in, and let’s get straight to the point.
Quick Answer
Short answer: Medicare may cover methoxsalen (both the oral capsule and the injectable form Uvadex) only when it’s part of a medically‑necessary phototherapy regimen – PUVA for severe psoriasis, or photopheresis for resistant cutaneous T‑cell lymphoma (CTCL). Coverage hinges on documented failure of standard treatments and proper paperwork.
Why does this matter? Because understanding the exact criteria can mean the difference between a denied claim and a smooth, reimbursed treatment plan.
What Is Methoxsalen
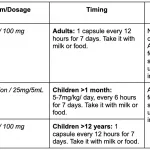
Methoxsalen, also known as 8‑MOP, is a type of psoralen – a light‑sensitive compound used to enhance the effects of ultraviolet (UV) therapy. You’ll see it under brand names like Oxsoralen (the oral capsule) and Uvadex (the injectable). Here’s how they’re typically used:
Oral Capsules – PUVA Therapy
Patients take a methoxsalen capsule about 1.5 to 2 hours before stepping into a UVA light chamber. The drug makes the skin temporarily more sensitive to UVA, allowing lower UV doses to clear stubborn plaques of psoriasis.
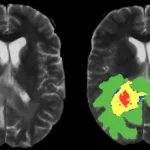
Injectable Uvadex – Photopheresis
Uvadex is mixed with a patient’s blood outside the body, exposed to UVA, and then reinfused. This “photopheresis” process is a targeted approach for hard‑to‑treat CTCL.
For a quick dive into the dosage details and safety profile, check out the official FDA label on DailyMed – Methoxsalen capsule.
Eligibility Rules
Medicare isn’t a free‑for‑all pharmacy. It pays for methoxsalen only when the treatment is deemed medically necessary. Here’s the breakdown.
General Medicare Requirements
- You must be enrolled in Medicare Part B (the part that covers doctor services and medical‑related drugs).
- The therapy must be prescribed after other standard options have failed.
- Your doctor must document the “intractable” nature of your disease.
CMS National Coverage Determination (NCD) for PUVA
The official policy, CMS NCD – Treatment of Psoriasis (250.1), states that PUVA (psoralen + UVA) is covered for “intractable, disabling psoriasis” after conventional therapies (topicals, UVB, coal‑tar) have been tried and found insufficient.
Uvadex & Photopheresis
There isn’t a stand‑alone CMS ruling for Uvadex, but many Medicare Administrative Contractors (MACs) treat it under the umbrella of “experimental/innovative therapy” for life‑threatening CTCL when extensive prior‑treatment failure is documented. A well‑crafted Letter of Medical Necessity can often tip the scales.
PUVA Details
What Medicare Pays For
When the claim is approved, Part B covers both the drug cost (HCPCS J3490) and the UVA phototherapy session (usually bundled under the same claim). You’ll typically see a 20 % coinsurance after the annual Part B deductible.
Time Limits
The NCD limits continuous PUVA coverage to 30 days unless your physician provides documented improvement. After 30 days, a new pre‑authorization is required.
Claim Flow – A Simple Table
| Step | What Happens |
|---|---|
| 1️⃣ Prescription | Dermatologist writes methoxsalen order with dosage and timing. |
| 2️⃣ MPD Test | Minimum Phototoxic Dose is measured; results attached to claim. |
| 3️⃣ Phototherapy Order | UVA unit scheduled; exposure time set per MPD. |
| 4️⃣ Billing | HCPCS J3490 + phototherapy code submitted to Medicare. |
| 5️⃣ Review | MAC checks documentation; approves or denies. |
Uvadex & Photopheresis
When It’s Covered
If you have CTCL that’s not responding to biologics, radiation, or systemic chemotherapy, photopheresis (Uvadex + UVA) can be a lifeline. Medicare will consider coverage when you can show:
- Pathology confirming CTCL stage II or higher.
- Documented failure of at least two other systemic therapies.
- A physician‑signed Letter of Medical Necessity referencing peer‑reviewed outcomes (e.g., a 2022 study in Blood on photopheresis efficacy).
Billing Tips
Use HCPCS J3490 for methoxsalen injection and the unlisted code E1399 for the photopheresis service, attaching a concise narrative that explains the diagnosis, prior treatments, and expected benefits.
How to Apply
Step‑by‑Step Guide
- Confirm Part B enrollment. Without it, the claim will bounce.
- Gather documentation. Pull together the physician letter, MPD results, prior‑therapy log, and any pathology reports.
- Submit a pre‑authorization. Your doctor’s office typically does this through the MAC’s online portal.
- File the claim. Include HCPCS codes, MPD documentation, and the treatment schedule.
- Monitor the status. If denied, you have 60 days to appeal—often just by adding the missing piece of paperwork.
Common Pitfalls (and How to Dodge Them)
- Missing MPD test. Medicare will flag the claim; get the test done before the first UVA session.
- Exceeding the 30‑day limit. Stop at 30 days, then request a continuation with new improvement data.
- Wrong HCPCS code. Double‑check J3490 for methoxsalen and E1399 for photopheresis; a typo leads to denial.
Benefits vs. Risks
Benefits
When covered, methoxsalen can be a game‑changer. PUVA often clears >70 % of plaques in 6 weeks, letting patients ditch painful creams and avoid systemic immunosuppressants. For CTCL, photopheresis can induce remission in patients who have exhausted other options.
Risks
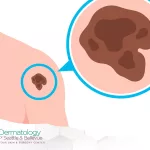
- Photosensitivity – you’ll need to avoid sunlight for 24 hours after a dose.
- Nausea or mild stomach upset (oral form).
- Long‑term increased skin‑cancer risk if UV exposure isn’t carefully controlled.
- Uvadex infusion reactions (rare, but possible).
Real‑World Example
John, 68, a Medicare beneficiary with severe plaque psoriasis, tried topical steroids, UVB, and biologics with little success. His dermatologist ordered a Minimum Phototoxic Dose test, documented the failed therapies, and submitted a pre‑authorization. Within two weeks, Medicare approved the PUVA regimen. Six weeks later, John reported a 70 % reduction in lesions and only a modest out‑of‑pocket coinsurance. His story underscores the power of thorough documentation.
Conclusion
Bottom line: Medicare can cover methoxsalen—but only when it’s part of a well‑documented, medically‑necessary phototherapy plan. Whether you’re pursuing PUVA for stubborn psoriasis or Uvadex + photopheresis for resistant CTCL, the key steps are: confirm Part B enrollment, get a solid MPD test, show that conventional treatments have failed, and keep the paperwork tight.
Feeling a little less overwhelmed? Good! Take this guide, share it with your dermatologist, and ask them to help you gather the required documents. If you’ve already gone through the process, we’d love to hear your story in the comments – your experience could help the next person in line.
Remember, you’re not alone in navigating Medicare’s maze. With the right information and a proactive approach, you can get the treatment you need without unexpected bills. If any part of this still feels fuzzy, drop a question below and let’s figure it out together.





















Leave a Reply
You must be logged in to post a comment.