Hey there! If you’ve ever wondered why the scale seems to have a mind of its own or felt a little uneasy hearing “overweight” tossed around, you’re not alone. Let’s cut through the noise, get straight to what matters, and give you a game‑plan that actually works. No jargon, no fluff—just friendly, real‑talk advice you can start using today.
Know Your Numbers
First things first: what does “overweight” really mean? The simplest way to tell is with the Body Mass Index (BMI). For adults, a BMI between 25 and 29.9 lands you in the overweight range. Anything 30 or above moves you into obesity territory. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), BMI is a quick screening tool—not a perfect measure, but it’s a solid starting point.
But don’t let a number scare you. Think of BMI as a friendly nudge, like a smartwatch reminding you to stand up. It’s also worth checking your waist circumference—over 40 inches for men or 35 inches for women adds extra risk, even if your BMI is borderline.
Health Risks
Now, why should you care? Because being overweight can raise the odds of several serious health problems. Here’s the quick rundown:
- Heart disease & hypertension – extra weight makes the heart work harder.
- Type‑2 diabetes – your body’s insulin gets less effective.
- Cancers – especially breast, colorectal, and endometrial.
- Sleep apnea – breathing troubles at night.
- Joint pain & osteoarthritis – more weight, more wear‑and‑tear.
- Mental health challenges – anxiety, depression, and lower self‑esteem.
These risks aren’t just abstract; they affect everyday life. Imagine feeling winded after climbing a single flight of stairs or having your doctor flag “elevated cholesterol” at each visit. The good news? Most of these risks can be softened—sometimes dramatically—with the right approach.
Treatment Options
Let’s talk solutions. There’s no one‑size‑fits‑all, but we can break it down into three tiers: lifestyle tweaks, medication, and—when needed—surgery.
Lifestyle First: Eating & Moving
Think of your body like a car. You wouldn’t pour sugar into the gas tank and expect it to run smoothly, right? A balanced, nutrient‑dense eating plan (think Mediterranean or DASH) is your premium fuel. Pair that with at least 150 minutes of moderate activity per week—walking, cycling, dancing, whatever gets your heart rate up.
If you’re curious about more specific steps, check out our guide on obesity treatment. It dives into practical meal planning, portion control, and sustainable activity ideas that won’t leave you feeling deprived.
Pharmacotherapy – GLP‑1 Agonists
For many, lifestyle changes alone move the needle only a little. That’s where GLP‑1 agonist medications shine. These drugs mimic a natural hormone that tells your brain you’re full, curbs cravings, and even improves insulin sensitivity.
Clinical trials show that people on GLP‑1 agonists can lose 10‑15% of their body weight within a year when combined with healthy habits. It’s not magic, but it’s a powerful tool that many doctors now prescribe as part of a comprehensive plan.
Emerging Option: Ecnoglutide Weight Loss
Enter ecnoglutide, a newer GLP‑1 style agent that’s been generating buzz. Early data suggest an average 15‑20% total body weight loss after 68 weeks—some of the most impressive results yet.
Because it’s still rolling out, talk to your healthcare provider about eligibility, insurance coverage, and potential side effects. The hype is real, but the science backs it up.
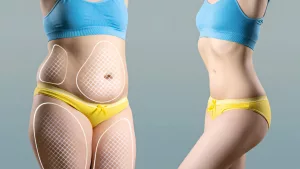
Surgical Interventions
If BMI is over 40—or over 35 with serious comorbidities—metabolic‑bariatric surgery becomes a consideration. Procedures like sleeve gastrectomy or gastric bypass can yield 25‑35% weight loss and often resolve diabetes or hypertension. It’s a major decision that demands thorough counseling, but for some, it’s life‑changing.
Quick Comparison
| Approach | Typical Weight Loss | Timeframe | Invasiveness |
|---|---|---|---|
| Lifestyle (diet + exercise) | 5‑10% | 6‑12 months | Low |
| GLP‑1 Agonist | 10‑15% | 12‑18 months | Low‑moderate (injection) |
| Ecnoglutide | 15‑20% | 18‑24 months | Low‑moderate (injection) |
| Bariatric Surgery | 25‑35% | 1‑3 years | High (surgical) |
Create Your Plan
Now that you’ve got the toolbox, let’s assemble a plan that fits your life.
Set Realistic Goals
Instead of “lose 30 pounds forever,” try “drop 5 pounds in the next month.” Use the SMART framework—Specific, Measurable, Achievable, Relevant, Time‑bound. Small wins build confidence and keep momentum alive.
Track, Adjust, Repeat
Keep a simple log: weight, waist measurement, how you felt that day, and any meds or foods you tried. Review weekly. If progress stalls, tweak a variable—maybe swap a sugary snack for a fruit, or add a 10‑minute walk after dinner.
Lean on Support
Whether it’s a friend, a family member, or an online community, sharing the journey makes it easier. Even a quick text saying “I’m hitting the gym at 7 am” can add accountability.
Mindful Eating
Slow down. Put your fork down between bites. Ask yourself, “Am I truly hungry, or am I bored?” Turning meals into a mindful ritual can curb over‑eating without feeling deprived.
Consider sustained weight reduction Strategies
Long‑term success hinges on habits that stick. Think of these as “maintenance tools” you keep in your kit: regular weigh‑ins, rotating fitness activities to stay excited, and periodic check‑ins with your doctor to adjust any meds if needed.
Real Stories
Stories help us see what’s possible. Here are two quick snapshots from folks who were once where you are now.
Maria’s Journey
Maria, 38, had a BMI of 28 and struggled with high blood pressure. She started with a modest 15‑minute evening walk and swapped soda for sparkling water. After three months, she added a GLP‑1 agonist prescribed by her endocrinologist. By month nine, she’d lost 18 % of her weight, and her blood pressure normalized. “I didn’t think a pill could be part of my plan, but it gave me the boost I needed while I built healthier habits,” she says.
James’s Turnaround
James, 45, tried countless fad diets with no lasting results. After a thorough evaluation, his doctor recommended ecnoglutide paired with a structured nutrition program. Six months later, James shed 22 % of his body weight, his sleep apnea resolved, and he could finally keep up with his teenage kids on the soccer field. “It felt like a team effort—my doctor, the medication, and my willingness to try new recipes,” James notes.
Take Action Today
Feeling a bit inspired? Great! Here’s a quick three‑step to‑do list you can start right now:
- Check your BMI. Use the CDC’s calculator and jot down your result.
- Pick one small habit. Maybe swap one sugary drink for water today, or add a 10‑minute walk after dinner.
- Schedule a chat. Book an appointment with your primary care provider to discuss whether a GLP‑1 agonist, ecnoglutide, or another obesity treatment option fits your needs.
Remember, you’re not alone in this. Every step—no matter how tiny—moves you toward a healthier, happier version of yourself. If you have questions, reach out to a trusted health professional, and keep the conversation going. We’re all in this together, cheering each other on.
What’s the first change you’re going to make today? Share your thoughts, try it out, and let’s celebrate every victory along the way.





















Leave a Reply
You must be logged in to post a comment.