Quick Answer
Gene‑edited pig kidneys have already functioned for more than a month inside brain‑dead humans, and a pig liver kept a patient alive for ten days without showing signs of rejection. Those early wins tell us that a pig‑to‑human transplant can be safe enough to move into real clinical trials, yet we still have a lot to learn about immune hurdles, long‑term durability, and the ethical questions that come with crossing species.
Why Pigs?
Imagine waiting years for a donor organ while your kidneys keep screaming for help. In the U.S. alone, over 100,000 people sit on the transplant list, and roughly 6,000 die each year before a match appears. That shortage makes the search for an abundant, compatible organ source feel almost desperate.
Pigs are surprisingly well‑suited for the job. Their organs are about the same size as ours, they reproduce quickly, and modern genetics lets us edit their DNA with precision. In short, they’re the closest match we have that can be produced at scale.
Genetic Tweaks
Knocking out the bad guys
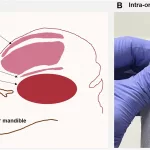
The human immune system is wired to attack anything it sees as foreign. Early xenotransplants flopped because the body recognized a sugar molecule called α‑Gal on pig cells and launched a hyper‑acute attack. By deleting the genes that create α‑Gal, as well as CMAH and B4GALNT2, scientists remove the main “red flags” that trigger that immediate rejection.
Adding human helpers
Even with the nasty sugars gone, pig organs can still set off other immune pathways. To calm things down, researchers insert human genes that act like peacekeepers: CD46, CD55, CD59 (which block complement), human thrombomodulin (which keeps blood clotting in check), and HLA‑E (which tells NK cells “I’m friendly”). The most advanced donor pigs now carry ten such edits – often called “10‑GE pigs.”
For a deeper dive into how these tweaks work, check out the recent review on the physiological basis for xenotransplantation.
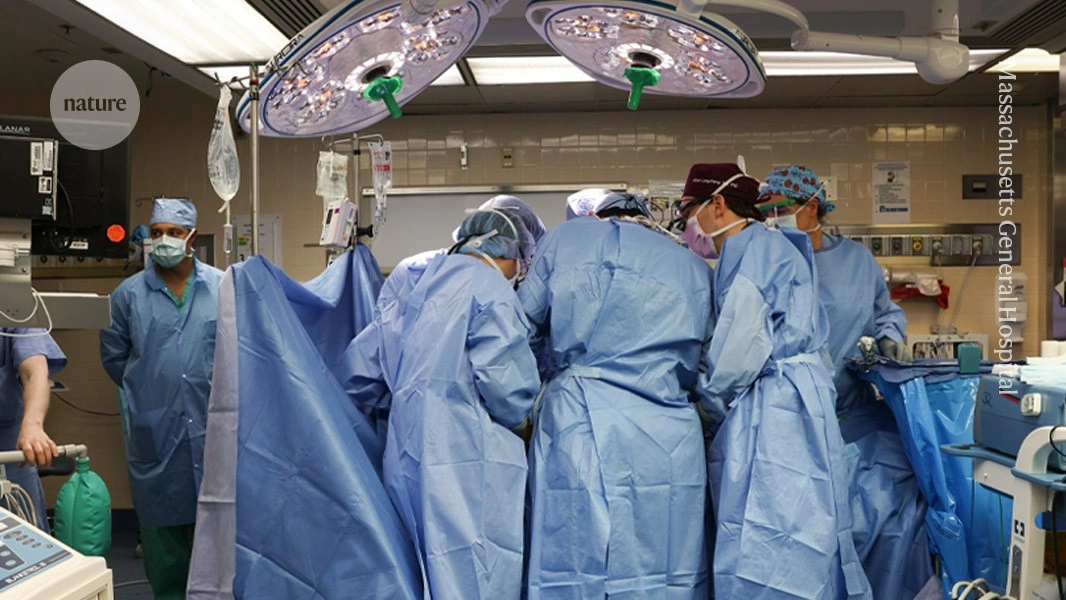
Clinical Milestones
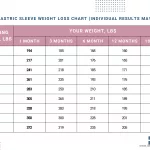
| Organ | Year | Model | Function/Survival | Key Take‑away |
|---|---|---|---|---|
| Kidney | 2023 | Brain‑dead human (NYU) | 32 days functional, no rejection | Single‑gene edit can sustain short‑term support |
| Kidney | 2024 | Brain‑dead human (UAB) | 7 days life‑sustaining | Proof of concept for longer grafts |
| Heart | 2022 | Living patient (Maryland) | 2 months survival | First clinical xenotransplant in a human |
| Liver | 2025 | Brain‑dead patient (China) | 10 days normal metabolism | First peer‑reviewed pig‑liver case |
Each of these studies tells a story of progress, but also of the nuanced challenges that still need solving. For example, the NYU kidney case required only one gene deletion, yet the patient needed a standard immunosuppression cocktail. The Chinese liver trial, meanwhile, showed that even a complex organ can avoid outright rejection when the donor pig is carefully screened for viruses.
Immune Response
From instant attack to chronic fire
When a pig organ first meets the human bloodstream, the body launches three main types of defense:
- Hyper‑acute rejection – driven by pre‑existing antibodies that recognize pig sugars.
- Acute cellular rejection – T‑cells and NK cells see the organ as “invader.”
- Chronic inflammation – a slower, smoldering response that can damage the graft over months.
Scientists monitor a set of xenotransplant markers to catch any trouble early. Typical markers include anti‑pig IgM/IgG titers, complement fragments (C3a, sC5b‑9), and cytokine spikes. When these rise, clinicians may adjust immunosuppressive drugs to keep the graft alive.
The human immune response to pig tissue
Even with the best genetic edits, the body still “recognizes” the organ as foreign. That’s why patients in the trials still receive drugs like tacrolimus, mycophenolate, and steroids. The good news? Because many of the most aggressive antigens are gone, the drug doses can often be lower than what’s needed after a traditional human kidney transplant.
Benefits vs Risks
What’s the upside?
- Unlimited supply – No more waiting lists if we can safely grow a herd of engineered pigs.
- Bridge therapy – A pig kidney could keep a patient alive while they wait for a perfect human match.
- Reduced organ mismatch – Gene edits can be tailored to specific HLA types, lowering the chance of rejection.
What could go wrong?
- Immune rejection – Even a tiny leftover antigen can spark a response.
- Zoonotic viruses – Pigs carry endogenous retroviruses; rigorous screening helps, but the risk isn’t zero.
- Long‑term durability – We’ve only watched pig kidneys survive weeks to a few months. Will they last a decade?
- Ethical concerns – Some patients and the public worry about “playing God” and the welfare of donor animals.
If you’re trying to weigh the pros and cons for a loved one, think of it like choosing a new car. A pig‑derived organ might be the only model on the lot right now, but you still want to check safety ratings, warranty length, and how it fits your lifestyle.
Regulatory Landscape
FDA’s compassionate‑use pathway
Since 2022, the U.S. Food and Drug Administration has allowed “compassionate‑use” cases for patients with no other options. The criteria are strict: the patient must be near‑terminal, the donor pig must be raised in a pathogen‑free facility, and the transplant team must have a detailed monitoring plan.
International rules
Europe, Japan, and China each have their own frameworks. The EU, for instance, bans germ‑line editing but permits somatic edits for xenotransplantation. China has moved quickly on clinical trials, especially for liver bridge support.
| Region | Key Regulation | Notable Milestone |
|---|---|---|
| United States | FDA compassionate‑use | 2022 pig‑heart case |
| European Union | EU Clinical Trial Regulation (CTR) | 2024 approved kidney pilot |
| China | National Health Commission guidelines | 2025 pig‑liver bridge study |
| Japan | Pharmaceuticals and Medical Devices Act | 2023 pre‑clinical primate work |
Future Directions
Trials on the horizon
By 2026 we expect Phase I/II kidney trials in the U.S., aiming to enroll 10‑15 patients with end‑stage renal disease who have been on dialysis for over five years. China is planning a version‑2 liver bridge study that will test whether a pig liver can support a patient for up to three weeks while a human organ is sourced.
Who might benefit?
Patients with rare blood‑type incompatibility, those who have been waiting longer than five years on dialysis, and individuals with contraindications to traditional immunosuppression (because pig organs may need less intense drugs) are the primary candidates. If you or someone you know fits that profile, it’s worth asking your transplant center about upcoming trials.
Questions to ask your doctor
- What specific gene edits does the donor pig have?
- How will my kidney transplant rejection risk be monitored?
- What infection‑screening protocols are in place for the pig donor?
- Will my immunosuppression regimen be different from a standard human‑to‑human transplant?
Conclusion
We stand at a remarkable crossroads where science, compassion, and technology intersect. The early successes of pig‑to‑human transplants—especially the steady function of gene‑edited kidneys and the surprising performance of a pig liver—show that we can move from “maybe someday” to “maybe today.” At the same time, the immune system’s stubborn vigilance, the lingering fear of hidden viruses, and the profound ethical questions remind us to tread carefully.
If you’re curious, hopeful, or even a little skeptical, keep the conversation going. Talk to your doctors, follow reputable news sources, and consider the personal stories of the brave volunteers who have already taken this step. Together, we can help turn the promise of pig‑to‑human transplantation into a reliable, life‑saving option for the millions waiting for a second chance.





















Leave a Reply
You must be logged in to post a comment.