Most people think addiction means “just one drug,” but when polysubstance use disorder is involved the brain and body are juggling two or more substances at the same time. That makes the warning signs harder to spot and the road to recovery a bit twistier. In the next few minutes you’ll learn what the disorder looks like, why it happens, which polysubstance treatment options actually work, and exactly what steps you can take today to get the dual‑diagnosis help you deserve—no endless scrolling required.
What Is Polysubstance?
Definition
Polysubstance use disorder (PUD) is a medical condition where a person regularly uses ≥ two different substances (including alcohol, prescription meds, or illicit drugs) within a 12‑month period and experiences significant impairment in daily life. The pattern meets the criteria for a substance‑use disorder even if no single drug, on its own, would qualify.
How DSM‑5 Treats It
The older DSM‑IV called this “polysubstance dependence.” The newer DSM‑5 folded it into the broader substance‑use disorder category, but clinicians still recognize the unique challenges of multiple‑drug use. According to Wikipedia, the shift reflects a deeper understanding that the combination of drugs can create a distinct clinical picture.
Common Substance Combinations
| Substance 1 | Substance 2 | Typical Effect | Primary Risk |
|---|---|---|---|
| Alcohol | Benzodiazepine | Deep sedation | Respiratory depression |
| Cocaine | Heroin | Intense “rush” then calm | Cardiac arrest |
| Prescription Opioid | Stimulant (e.g., meth) | Balancing high/low | Seizures, overdose |
| Cannabis | Alcohol | Heightened euphoria | Impaired judgment |
Spotting the Signs
Core Symptoms
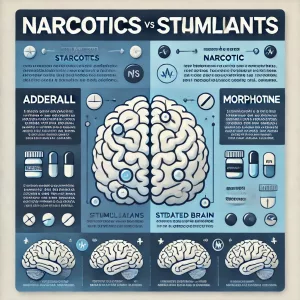
Because multiple drugs are involved, the classic “craving, tolerance, withdrawal” trio shows up in different guises. You might notice a strong urge to use both a stimulant and a depressant within the same day, escalating doses of each to chase the same feeling, or a constant cycle of seeking the next high.
Red‑Flag Behaviors Unique to PUD
- Mixing prescription painkillers with alcohol and not realizing the danger.
- Switching from a “upper” (cocaine, meth) to a “downer” (benzos) in a single afternoon.
- Using one drug to “smooth out” the side effects of another (e.g., benzodiazepines to ease opioid withdrawal).
Dual Diagnosis Overlap
Many folks with PUD also wrestle with anxiety, depression, or trauma. The co‑occurring mental‑health issue can fuel the urge to self‑medicate, creating a vicious loop. Recognizing that the mood swings or panic attacks may be part of a larger picture is essential for effective treatment.
Why Multiple Drugs?
Biological & Genetic Influences
Family history matters. If a parent struggled with addiction, your brain’s reward pathways may be wired to chase pleasure more aggressively. Studies show a higher prevalence of PUD among people with a genetic predisposition to substance dependence.
Environmental Triggers
Growing up in a household where several substances are present, or hanging out in circles where “mixing” is the norm, can make poly‑use feel like the default way to have fun. Early exposure to any drug dramatically raises the odds of later polysubstance patterns.
Psychological Motives
Enhancement: “I want a bigger, faster high.” Mixing alcohol with a benzodiazepine, for instance, multiplies the sedative effect.
Counter‑action: “I need a boost after the crash.” A stimulant may be taken to shake off the drowsiness from a prior opioid dose.
Both motives can be compelling, especially when the brain is desperate for relief.
Demographic Trends
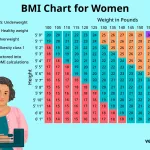
Data from the CDC shows that males, adolescents, and people who start using before age 18 are most likely to develop polysubstance use disorder. The earlier the exposure, the more entrenched the pattern becomes.
Getting Proper Diagnosis
What Clinicians Look For
Doctors use structured interviews that align with DSM‑5 criteria, ask about all substances (including over‑the‑counter meds and herbs), and often confirm with urine or blood screens. Honest disclosure is key—hiding one drug can skew the whole picture and delay proper care.
Screening Tools
Tools such as the Alcohol Use Disorders Identification Test (AUDIT), Drug Abuse Screening Test (DAST), and a dedicated polysubstance module help pinpoint the extent of multi‑drug use. When combined with a medical exam, they give a clear roadmap for treatment.
Finding a Qualified Program
If you’m ready to look for help, the SAMHSA treatment locator is a trustworthy place to start. According to SAMHSA, you can filter for “polysubstance” programs that offer integrated medical and behavioral care.
Treatment Options
Medical Detox – Why It’s Critical
Detoxing from one drug is already uncomfortable; withdrawing from several at once can be dangerous. Supervised detox monitors vital signs, balances medications for each substance, and prevents complications like seizures or severe alcohol withdrawal. Many centers give thiamine and folic acid prophylactically—simple vitamins that can dramatically reduce the severity of alcohol‑related delirium.
Integrated Psychotherapy
Cognitive‑Behavioral Therapy (CBT) helps you spot triggers for each drug class and develop healthier coping skills. Motivational Enhancement Therapy (MET) sparks internal desire to change, especially when the decision to quit feels overwhelming. For folks with co‑occurring mental‑health issues, dual‑diagnosis counseling treats both the substance pattern and the underlying mood disorder simultaneously.
Medication‑Assisted Treatment (MAT)
MAT isn’t just for opioids. Buprenorphine‑naloxone can calm opioid cravings while a low‑dose gabapentin eases withdrawal from alcohol and benzodiazepines. Recent research published in JAMA Psychiatry (2023) shows that combining MAT with behavioral therapy cuts relapse rates for people using both opioids and stimulants.
Aftercare & Community Support
Recovery doesn’t end at discharge. Twelve‑step groups that welcome “multi‑drug” members, sober‑living homes, and tele‑therapy check‑ins keep you accountable. Peer recovery coaches who have walked the same path can share practical tips—like how to handle the urge to “just have a drink” after a stressful day.
First‑30‑Day Recovery Checklist
- Attend at least three therapy sessions (CBT or MET).
- Take prescribed MAT exactly as directed.
- Log every substance you used in the past month.
- Reach out to a support person daily.
- Schedule a follow‑up medical check‑up before week 4.
Real‑World Success
Short Personal Narrative
When I first heard about “Jake,” a 28‑year‑old who mixed oxycodone, whiskey, and benzodiazepines, I imagined a hopeless spiral. In reality, Jake entered a specialized polysubstance program, detoxed under medical supervision, and spent six weeks in intensive CBT. Today he describes his life as “stable enough to enjoy a coffee without counting drinks.” His story reminds us that change is possible, even when the problem feels massive.
Clinician Spotlight
Dr. Maya Patel, an addiction psychiatrist with two decades of experience, says, “Treating PUD is like juggling multiple balls. If you focus on only one, the others keep bouncing back. Integrated care—where medical, psychiatric, and behavioral teams speak the same language—is the only way to catch them all.” Her insight underscores why a coordinated approach beats piecemeal solutions.
Take Action Now
Feeling a little uneasy after reading all this? That’s normal. The first step is simply becoming aware that you—or someone you love—might be dealing with a complex pattern of use.
- Self‑Screen: Answer a quick set of “yes/no” questions about cravings, mixing, and daily functioning. Many reputable sites offer a free, confidential assessment.
- Write It Down: List every substance you’ve taken in the past month, including alcohol, caffeine, OTC meds, and even herbal supplements.
- Reach Out: Call a trusted helpline or schedule a tele‑visit with an addiction specialist. A short conversation can reveal hidden risks.
- Tell a Support Person: Share your list with a friend, family member, or counselor who can help you stay accountable.
- Start a Recovery Journal: Document cravings, triggers, and small victories. Seeing progress on paper can be incredibly motivating.
Remember, you don’t have to face this alone. Professional help, compassionate friends, and evidence‑based treatment together create a sturdy bridge from chaos to stability.
Conclusion
Polysubstance use disorder is a distinct, high‑risk condition that blends the symptoms, causes, and treatment needs of several drugs into one “multiple‑drug addiction.” Recognizing the red‑flags early, obtaining a thorough diagnosis, and pursuing an integrated polysubstance treatment plan—often involving dual‑diagnosis help—greatly improve the odds of lasting recovery. If anything in this article feels familiar, don’t wait: reach out to a qualified professional today and take the first concrete step toward a clearer, healthier future.






















Leave a Reply
You must be logged in to post a comment.