
Your Teeth, Your Heart, Your Worries
Picture this: You finally call your dentist for that tooth extraction you’ve been putting off forever. No big deal, right? But in the middle of all the appointment reminders and anxiety about drills… that uneasy question pops in your head—what about the blood thinners you take religiously for your heart?
Maybe it was your last heart check-up, or maybe a scary news story you overheard at the pharmacy, but suddenly you’re thinking: “Am I supposed to just stop blood thinner before removing tooth? What’s the ‘right’ thing here?” It’s not a little thing… Bleeding, clots, strokes… It feels like a big deal because it honestly is. If this is where you are, you’re not alone. I’m not a dentist, but I’ve navigated this exact gauntlet with my dad—not that long ago. (Spoiler: He’s doing just fine, no ER visits, and his new smile is epic.) Let’s sit down, grab a coffee (decaf if you want to be extra healthy), and hash this out together—no stress, no fluff, no guilt.
Why Blood Thinners Are a Love-Hate Relationship
Ever catch yourself resenting your blood thinner prescription? You know, that tiny pill you love for being the superhero against clots, but can’t stand because it turns every paper cut into a murder scene. It’s like a double-edged sword—protects your heart, but oh wow, makes even a hangnail look dramatic. Blood thinners (the fancy folks call them anticoagulants or antiplatelets) make your blood less “sticky.” This stops clots from lurking and causing big disasters, like stroke, heart attack, deep vein thrombosis, and so on. For many of us, skipping isn’t really an option—not without some scary roulette happening in your body.
But what nobody tells you when you get the prescription is what you’re supposed to do when something “invasive” comes up, like—you guessed it—a tooth extraction. It’s like your best friend showing up to a pool party wearing full winter gear. Necessary… but awkward.
So… Do You Really Need to Stop?
I’ll be honest: The answer isn’t as simple as a yes or a no. (Aren’t grown-up answers always that way?) There’s this myth floating around—”You have to stop blood thinner before removing tooth.” I’ve heard it a hundred times in waiting rooms and at family BBQs. But want the honest scoop straight from people in the know? According to the American Dental Association, for most healthy-ish folks, you usually do not need to stop your blood thinner for a single, routine tooth extraction or minor dental surgery. They even have a whole protocol for dentists to follow to keep bleeding in check using local tricks (according to the ADA’s recommendations).
So why all the fuss? Because, like every good plot twist, there are exceptions. Risks. And your personal story and medical team matter—a lot. It’s never “one size fits all.”
Real Life: My Dad, His Warfarin, And The Great Tooth Rescue
Confession: The first time my dad needed a tooth pulled on warfarin, my mom was convinced he’d bleed buckets. She panicked. She researched. She panicked some more. We called his dentist, who told us, “No, don’t abruptly stop! Let’s talk to your heart doctor.” Then together, they checked his INR (a measure of how slow/fast his blood clots on the medication). They also looped in a fancy mouthwash and special packing for the extraction… and guess what? He went home the same day, telling bad jokes like nothing happened. We learned that team communication is everything… and not to trust Internet horror stories without double-checking.
Tug-Of-War: To Stop, Or Not?
Okay, let’s get honest. Why is this even a debate? Because stopping blood thinners isn’t just about less bleeding. It can mess with the entire reason you’re on those meds: avoiding strokes, clots, major heart drama. If you pause them cold-turkey, you could flip the risk script. Yeah, stopping might mean less oozy gums… but it might also mean a trip to the ER for something scarier. (Not worth it!)
On the flipside, not stopping can mean a bit more blood than “normal.” But here’s a secret: Most dental teams are absolute pros at managing bleeding. They use little collagen sponges, extra sutures, and sometimes nifty solutions like tranexamic mouthwash. Bleeding is usually mild and controlled—not epic movie-level drama. Serious bleeds are rare if your team plans ahead. Local research on oral anticoagulants and tooth extractions repeats this over and over (see the clinical recommendations here).
So… What’s The Catch?
If you have a high-risk medical situation—multiple health issues, a history of wild bleeding, or you’re getting a bunch of teeth pulled—it could be smart to pause or adjust your dose, but ONLY with your doctors’ help. No exceptions! For some meds (like certain doses of warfarin or when doing more complex extractions), they might suggest holding the med for a day or two. Or, with “newer” blood thinners like When to stop Eliquis before tooth extraction, your team will time things out based on your prescription and kidney function. You don’t have to memorize the science—just tell your dentist everything. (If you forget, your body will probably remind you. There will be blood…)
Blood Thinners: Old vs. New
Here’s something you may not have heard before… Not all blood thinners play by the same rules. “Old school” ones—like warfarin—need frequent finger pricks, and the safe “zone” is narrow. For these, we talk about something called INR (International Normalized Ratio). If it’s too high, you bleed; too low, you clot. Newer meds, like Eliquis or Xarelto, usually don’t need as much blood testing and their effect wears off faster if you stop. Sometimes the timing is as simple as “miss one dose, then restart,” but only your doctor knows for sure.
| Type | Examples | Need To Stop? | Special Tips |
|---|---|---|---|
| Old school | Warfarin (Coumadin) | Rarely, if INR is safe | Test blood before; never stop on your own |
| Newer | Eliquis, Pradaxa, Xarelto | Uncomplicated extractions—often no stop needed | Let doc plan timing; check When to stop Eliquis before tooth extraction for details |
If you take aspirin, Plavix, or other antiplatelet meds, the story is similar—a team approach, not a solo gamble. The joys of modern medicine, right?
What Do Real-Life Dentists Actually Do?
I asked Dr. Kim (okay, I cornered her at the school charity 5K) what she does when a patient calls in a freak-out: “We check your whole history, call your heart doctor, maybe order blood work, and build a little ritual to keep you safe. Sometimes we use magic mouth rinses or extra-absorbent packing. Usually, I’m more worried about you biting your cheek after than bleeding out!” It made me laugh—she’s seen hundreds of these cases. Bleeding is almost always manageable with extra planning.
According to research on dental extractions (think ridge oral surgery’s protocol), the secret is communication between your health squad. Cute takeaway from Dr. Kim: “Always tell your dentist which blood thinner you’re on, how much, and why. Never stop on your own. Call first. Save yourself the stomach aches, the what-ifs, and the Dr. Google rabbit holes.”
Step-By-Step: What Actually Happens
Okay, nuts and bolts time. Here’s what usually happens if you walk into your dentist’s office, blood thinners in tow:
- You tell your dentist what meds you’re on—by name, dose, and frequency. (Don’t be shy. Even scribbled on a napkin is fine.)
- Your dentist calls your heart/care doctor. They look at your latest test results and assess risk. This is standard—don’t feel awkward.
- If you’re on warfarin, they’ll check your INR. If you’re on newer meds, it’s about timing with your dosage.
- They’ll set up extra safety—early morning appointments, special mouthwashes, more time to clot, maybe tranexamic acid rinse (sounds fancy, but it helps keep bleeding tame).
- If you have a wild medical history or several teeth to be pulled, you might get a med adjustment—but never without a plan. You’ll have your full medical team on this journey. Kind of like a pit crew for your smile.
An Extra Story: The “Scary” Bleeder Who Was Totally Fine
I once met a runner at a nutrition talk who needed both a tooth out and was on Eliquis. She was petrified she’d bleed for days. Her oral surgeon assured her—no need to stop the med, but they’d double up on pressure packs and keep her for an extra half hour to make sure she clotted. That was it. She called it “shockingly boring”—and isn’t that what we want from medical procedures?
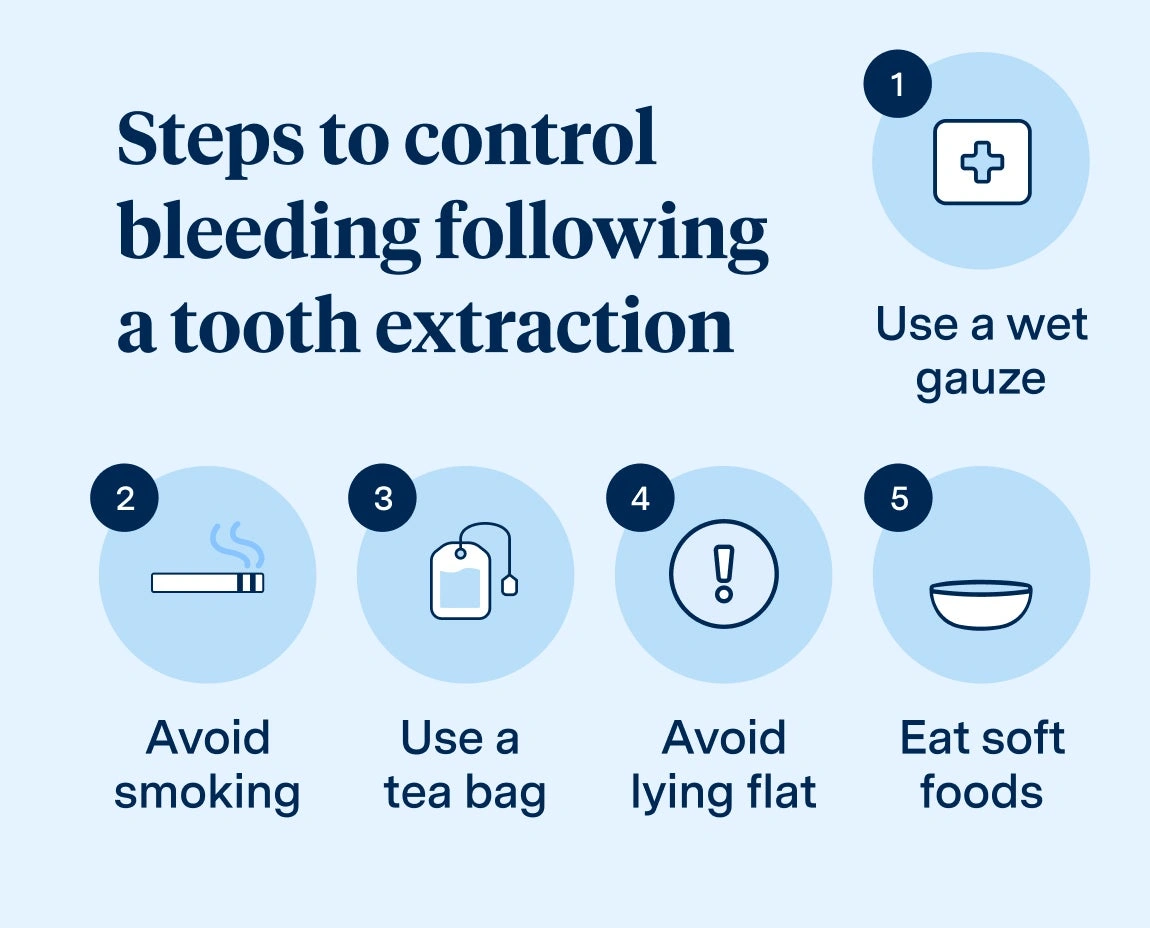
But What About After The Extraction?
Ah yes—the “what next?” phase. So picture this: You’ve made it through the extraction, and now you’re staring at your mouth in the mirror, trying to decide if it’s “normal” to see a little red. (Hint: yes!) Here’s what to expect:
- Slight bleeding, oozing, or pink saliva is normal for a few hours. If it looks like the set of a horror movie—call your dentist, but don’t freak yet.
- Do the soft food thing: Yogurt, oatmeal, ice cream if you’ve got an excuse. (No judgment.)
- Avoid heavy lifting, gym sessions, or blowing up beach balls in the first 24 hours. (Ask me how I learned this one… I emptied a socket on a hike. Fun times.)
- Expect your dentist or surgeon to call you or check in—especially if you’re on blood thinners. If bleeding picks up or you get dizzy—call them, stat.
Most people (statistically more than 95%) are back to normal the next day or two. Medical science and teamwork for the win.
What’s The Bottom Line? Your Safety Checklist
Let’s just pop some highlights into your back pocket:
- Never stop blood thinner before removing tooth unless your health team says it’s safe and necessary.
- Tell your dental team about every blood thinner and any health condition, even if you think it’s not important.
- Get all your aftercare instructions in writing—and follow them. Don’t improvise.
- If you’re nervous or have a unique situation, bring a loved one or friend for the consult. Extra eyes and ears never hurt.
- For Eliquis (and similar meds), see the latest advice and timing at When to stop Eliquis before tooth extraction.
No superheroes here… just teamwork, transparency, and a friendly nudge to reach out if you’re ever unsure.
Ready To Face That Extraction? You’ve Got This.
Breathe out for a second. You’re smarter already for reading this. Here’s the gentle truth: Tooth extractions and blood thinners go together more easily than you might think—if you communicate, trust your team, and don’t play amateur pharmacist. For most people, the safest thing is actually not to pause those clot-busters unless your doctor says so. Serious complications from uncontrolled bleeding or clotting are rare these days—but only if you don’t guess, don’t Google DIY, and don’t hide your meds. Start by telling your dentist everything, planning together, and trusting the process. For more personal stories, up-to-date tips, and honest advice, check out stop blood thinner before removing tooth. If you like rabbit holes, or you’re specifically dealing with Eliquis, the details at When to stop Eliquis before tooth extraction are life-savers.
Seriously—don’t let a little (or a lot) of worry keep you from a healthy mouth and a strong heart. What would make it easier for you to schedule that appointment? Share your story below, or pass this along to a friend who’s putting off care. Here’s to fewer “what ifs,” more peace of mind, and one less thing weighing on your shoulders.






















Leave a Reply
You must be logged in to post a comment.