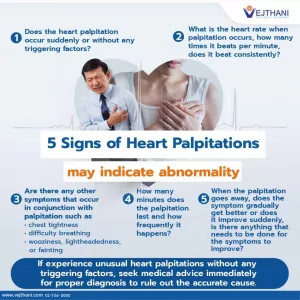
Cholesterol is a waxy substance your body requires to manufacture certain hormones and to form the outer membrane of every cell. While some cholesterol is necessary, excess amounts can accumulate in your blood vessels and increase your chances of:
- heart disease
- stroke
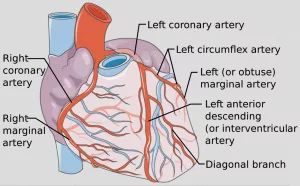
- atherosclerosis, a narrowing or stiffening of your arteries
The recommendations advise starting cholesterol screening in childhood or adolescence and repeating tests at least every 5 years after age 20.

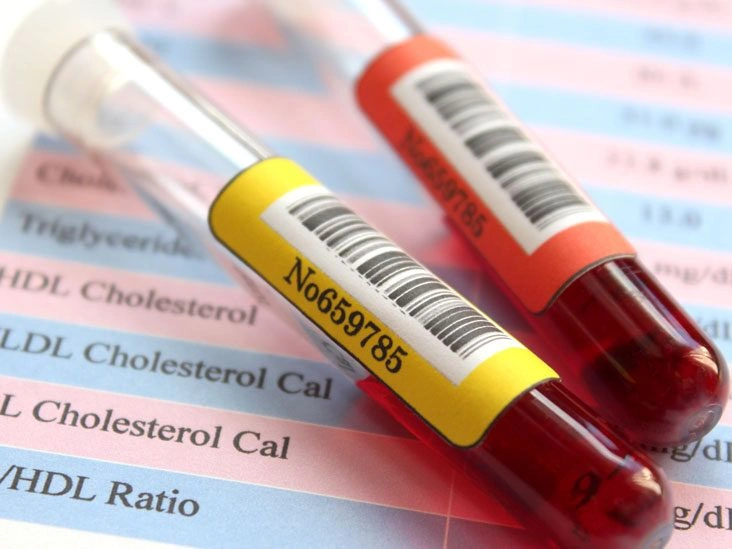
What does a cholesterol test measure?
A full cholesterol test, often called a lipid panel or lipid profile, evaluates the concentrations of lipids, or fats, in your bloodstream. It mainly assesses your:
- High-density lipoprotein (HDL) cholesterol. HDL is known as “good” cholesterol because it helps remove LDL cholesterol from your bloodstream.
- Low-density lipoprotein (LDL) cholesterol. LDL is labeled “bad” cholesterol. Elevated LDL can cause cholesterol to deposit on artery walls, increasing the risk of heart attack, stroke, and atherosclerosis.
- Triglycerides. After you eat, your body breaks dietary fats into molecules called triglycerides. Elevated triglyceride levels increase cardiovascular disease risk. Obesity, uncontrolled diabetes, excessive alcohol use, and a high-calorie diet can all raise triglyceride levels.
- Very low-density lipoprotein (VLDL). Another cholesterol-related particle in your blood is VLDL. Labs typically don’t measure VLDL directly; instead, VLDL is estimated based on a proportion of triglyceride levels. VLDL values generally aren’t used to guide treatment for high cholesterol.
- Total cholesterol. This represents the overall cholesterol in your blood, the sum of LDL, HDL, and VLDL. Total cholesterol and HDL are directly measured; LDL and VLDL are calculated from total cholesterol, HDL, and triglyceride measurements.
What’s considered a normal range?
In the U.S., cholesterol and triglyceride values are reported in milligrams (mg
Cholesterol is a waxy substance your body requires to manufacture certain hormones and to form the outer membrane of every cell. While some cholesterol is necessary, excess amounts can accumulate in your blood vessels and increase your chances of:
- heart disease
- stroke
- atherosclerosis, a narrowing or stiffening of your arteries
The recommendations advise starting cholesterol screening in childhood or adolescence and repeating tests at least every 5 years after age 20.

What does a cholesterol test measure?
A full cholesterol test, often called a lipid panel or lipid profile, evaluates the concentrations of lipids, or fats, in your bloodstream. It mainly assesses your:
- High-density lipoprotein (HDL) cholesterol. HDL is known as “good” cholesterol because it helps remove LDL cholesterol from your bloodstream.
- Low-density lipoprotein (LDL) cholesterol. LDL is labeled “bad” cholesterol. Elevated LDL can cause cholesterol to deposit on artery walls, increasing the risk of heart attack, stroke, and atherosclerosis.
- Triglycerides. After you eat, your body breaks dietary fats into molecules called triglycerides. Elevated triglyceride levels increase cardiovascular disease risk. Obesity, uncontrolled diabetes, excessive alcohol use, and a high-calorie diet can all raise triglyceride levels.
- Very low-density lipoprotein (VLDL). Another cholesterol-related particle in your blood is VLDL. Labs typically don’t measure VLDL directly; instead, VLDL is estimated based on a proportion of triglyceride levels. VLDL values generally aren’t used to guide treatment for high cholesterol.
- Total cholesterol. This represents the overall cholesterol in your blood, the sum of LDL, HDL, and VLDL. Total cholesterol and HDL are directly measured; LDL and VLDL are calculated from total cholesterol, HDL, and triglyceride measurements.
What’s considered a normal range?
In the U.S., cholesterol and triglyceride values are reported in milligrams (mg) of cholesterol per deciliter (dL) of blood.
If your cholesterol readings fall outside the normal range, your risk for heart disease, stroke, and atherosclerosis may be higher.
Your clinician will factor in other elements, like family history, body weight, and activity level, to evaluate your risk.
If results are abnormal, your provider may request a blood glucose test to screen for diabetes and possibly a thyroid function test to check for underactive thyroid.
Can test results be wrong?
Occasionally, cholesterol test results can be inaccurate. For instance, research has shown that assuming VLDL equals 20 percent of triglyceride levels becomes less reliable when triglycerides exceed 400 mg/dL.
Incorrect fasting, certain medications, human mistakes, and other variables can lead to false-negative or false-positive outcomes.
Measuring both HDL and LDL typically yields more dependable results than assessing LDL alone.
Who should have a cholesterol test?
Cholesterol screening is particularly important if you:
- have a family history of high cholesterol or heart disease
- are overweight or obese
- consume alcohol frequently
- smoke cigarettes
- have a sedentary lifestyle
- have diabetes, kidney disease, polycystic ovary syndrome, or an underactive thyroid
The CDC advises routine testing every 4–6 years for most healthy adults. Those with a family history of high cholesterol or other risk factors may need more frequent checks.
The CDC also recommends that children, teens, and young adults have cholesterol checked once between ages 9 and 11 and again between 17 and 21.
Preparation for a cholesterol test
Sometimes your clinician may ask you to fast before a cholesterol test.
However, according to 2018 guidelines in the Journal of the American College of Cardiology, a nonfasting test can reliably detect high cholesterol or lipid abnormalities in adults over 20 who are not on lipid-lowering medications.
If fasting is required, avoid eating or drinking anything except water for 9 to 12 hours before the blood draw.
Before testing, inform your clinician about:
- any symptoms or health concerns you have
- your family’s heart health history
- all medications and supplements you take
If you take medicines that might raise cholesterol — such as certain oral contraceptives — your clinician may advise stopping them several days prior to the test.
How is a cholesterol test performed?
To assess cholesterol, a blood sample is collected, usually in the morning and sometimes after an overnight fast.
A blood test is an outpatient procedure that takes only a few minutes and is generally minimally painful. It’s commonly done in a diagnostic laboratory but can also be performed during a routine doctor visit, at a pharmacy, or at home.
Walk-in clinic fees often range from $50 to $100. Pharmacy cholesterol screenings can cost $5 to $25. At-home tests may cost $15 to $25, while mail-in kits that require lab processing average $75 to $200.
If a physician orders the cholesterol test, health insurance typically covers it fully or partially.
Risks from having blood drawn are minimal. You might feel lightheaded or have soreness at the puncture site, and there is a very small risk of infection where the needle was inserted.
Are home cholesterol tests reliable?
Accuracy varies among home cholesterol test brands and depends on how closely you follow the instructions.

In a study, researchers found that two point-of-care lipid devices were fairly accurate and met industry standards. They reported that:
- HDL readings were within 12 percent of laboratory results.
- Total cholesterol was within 10 percent.
- Triglyceride values were within 15 percent.
In another analysis, investigators reviewed five commercial home cholesterol tests. They determined that the Roche Accutrend Plus performed excellently, while several other products showed poor accuracy and diagnostic capability.
Researchers concluded that improved regulation and standardization are necessary for at-home cholesterol testing.
For the most dependable results, lab-based testing may still be the preferred choice, especially if you have risk factors for elevated cholesterol.
Lifestyle changes and treatment
Elevated cholesterol can be managed through lifestyle adjustments and medication. Reducing LDL often helps lower the risk of heart disease and related problems.
To help lower harmful cholesterol:
- If you smoke, consider quitting. Discuss with your clinician a smoking cessation strategy that suits you.
- Eat a balanced diet. Emphasize mostly unprocessed foods, a variety of vegetables and fruits, whole grains, low-fat dairy, and lean protein. Increase soluble fiber intake and limit foods rich in saturated fats, like butter, cream, fatty meats, and palm oil.
- Avoid trans fats. Artificial trans fats are detrimental to heart health. Read labels and avoid products listing partially hydrogenated oils.
- Exercise regularly. Aim for at least 150 minutes of moderate-intensity aerobic activity weekly, which averages about 22 minutes per day.
- Maintain a healthy weight. Excess body weight is a major risk factor for high cholesterol. Talk with your clinician about an appropriate weight range for you.
- Limit alcohol intake. Heavy drinking raises the risk of many conditions, including heart disease, high cholesterol, liver disease, and certain cancers.
Your clinician may recommend a “therapeutic lifestyle changes” (TLC) diet. This plan suggests that no more than 7 percent of your daily calories come from saturated fat and limits dietary cholesterol to under 200 mg per day.
Certain foods can reduce cholesterol absorption in the gut. Your clinician may suggest eating more:
- oats, barley, and other whole grains
- fruits like apples, pears, bananas, and oranges
- vegetables such as eggplant and okra
- beans and legumes including kidney beans, chickpeas, and lentils
If lifestyle changes alone don’t sufficiently lower cholesterol, your clinician may prescribe medications such as statins to reduce LDL levels.
Learn more about lowering your cholesterol here.
The bottom line
A cholesterol test evaluates cholesterol and fat levels in your blood to help gauge cardiovascular risk.
Most healthy adults should have cholesterol checked at least every 5 years. Those with a family history or elevated risk should be tested more frequently.
If you have high cholesterol, your clinician can develop a treatment plan to bring levels into a healthy range.
Treatment typically involves some combination of dietary changes, more physical activity, quitting smoking, and medication.




















Leave a Reply
You must be logged in to post a comment.