Most people don’t realize that treating type 1 diabetes really boils down to three simple ideas: insulin, technology, and lifestyle. If you’re wondering how to keep your blood sugar steady without feeling like you’re on a never‑ending roller coaster, you’re in the right place. In the next few minutes we’ll break down everything you need to know—plainly, with a dash of humor, and a lot of empathy—so you can feel confident about your treat type 1 diabetes plan.
Core Treatment
What Is Insulin and How Does It Work?
Think of insulin as the key that unlocks the door to your cells, letting glucose (the fuel you eat) in to power everything from a morning jog to a Netflix binge. In type 1 diabetes the pancreas stops making that key, so you have to provide it yourself.
Quick Physiology
When carbs break down into glucose, insulin binds to receptors on cell surfaces, prompting glucose transporters to swivel open. Without insulin, glucose stays stuck in the bloodstream, turning numbers on your meter red and eventually causing long‑term damage.
Types of Insulin
There are four main families, each with its own “speed” and “duration.” Below is a handy cheat‑sheet you can print and stick on your fridge.
| Insulin Type | Onset | Peak | Duration |
|---|---|---|---|
| Rapid‑acting (e.g., Humalog, NovoLog) | 5‑15 min | 1‑2 hr | 3‑5 hr |
| Short‑acting (Regular) | 30‑60 min | 2‑4 hr | 5‑8 hr |
| Intermediate (NPH) | 1‑3 hr | 4‑12 hr | 12‑18 hr |
| Long‑acting (Lantus, Tresiba) | 1‑2 hr | None (steady) | 24‑42 hr |
According to Diabetes UK, mixing a long‑acting basal insulin with a rapid‑acting bolus before meals mimics the pancreas’s natural pattern and is the gold standard for most adults.
How Doctors Design a Personalized Insulin Plan
Every body is a different engine. Your endocrinologist will work with a certified diabetes educator (CDE) and a dietitian to set up a “basal‑bolus” routine—think of basal as the cruise control and bolus as the gas pedal when you eat.
Basal‑Bolus Concept
Basal insulin keeps blood sugar stable between meals and overnight. Bolus insulin handles the rise that follows carbs. The ratio of insulin‑to‑carb (often “1 unit per 10‑15 grams of carbs”) is unique to you and may shift as you grow, exercise, or get sick.
Teamwork Makes the Dream Work
Don’t underestimate the power of a supportive care team. A single conversation with a knowledgeable CDE can save you from countless hypoglycemia scares.
Insulin Options
Injections vs. Pens vs. Pumps
When I first switched from syringes to a pen, it felt like upgrading from a flip phone to a smartphone. The difference is in the details: precision, convenience, and comfort.
Pros & Cons
- Syringes: cheap, but can be fiddly and painful.
- Insulin pens: discreet, dose‑accurate, slightly more expensive.
- Pumps: deliver tiny “basal” bursts continuously, reduce hypos, but require a learning curve and insurance approval.
When a Pump Is Worth It
If your A1C stays above 7 % despite diligent effort, or you experience frequent lows, a pump may be the answer. The NHS says pump eligibility includes “inability to reach target glucose levels without serious hypoglycemia” (NHS).
Closed‑Loop / Hybrid Systems (Artificial Pancreas)
Imagine a tiny robot that reads your glucose numbers every five minutes and nudges insulin out of a pump to keep you steady. That’s a closed‑loop system, also called an artificial pancreas.
How It Works
A continuous glucose monitor (CGM) sends data to an algorithm, which then tells the pump how much insulin to dispense. The loop runs automatically, but you still play a role in confirming meals and exercise.
Real‑World Outcomes
A 2024 study in the Journal of Diabetes Science showed a 0.5 % drop in A1C and 30 % fewer severe hypoglycemia episodes for users of hybrid systems versus traditional injections (a study reported by the American Diabetes Society). That’s a big win for peace of mind.
Glucose Monitoring
Why CGM Is a Game‑Changer
When you used to finger‑prick six times a day, a CGM feels like swapping a dial‑up connection for fiber‑optic. Real‑time readings, trend arrows, and low‑glucose alarms empower you to catch problems before they become emergencies.
CGM‑Only vs. CGM + Pump
If you love the freedom of a pump, pair it. If not, a standalone CGM still gives you insight into daily patterns—think of it as your personal glucose diary you don’t have to write.
Choosing the Right Device
Consider sensor lifespan (7‑14 days), need for calibration, and insurance coverage. The Diabetes UK checklist is a solid starting point: does it integrate with your phone? Does it alert you when glucose drops?
Nutrition Basics
Carb Counting for Insulin Dosing
Carb counting is the language your insulin speaks. If you know “10 g of carbs = 1 unit of rapid‑acting insulin,” you can match insulin to food with confidence.
How to Calculate Your Ratio
Start with a test day: track carbs and insulin doses, then look at resulting glucose trends. Most adults end up with a ratio of 1 unit per 10‑15 g carbs. Your dietitian can fine‑tune this.
Free Apps Suggested by Experts
My favorite? mySugr and CarbCount. Both sync with popular CGMs and make the math feel like a game.
What to Eat (and What to Limit)
Think of your plate as a balanced orchestra:
- Proteins: lean meats, beans, tofu—steady energy.
- Healthy Fats: avocados, nuts, olive oil—slow glucose rise.
- Low‑Glycemic Carbs: non‑starchy veg, berries, whole grains.
- High‑Glycemic Treats: reserve for “bolus‑friendly” moments with extra insulin.
Sample Day
| Meal | Food | Carbs (g) | Insulin (U) |
|---|---|---|---|
| Breakfast | Greek yogurt + ½ cup berries + 1 slice whole‑grain toast | 30 | 2 |
| Lunch | Grilled chicken salad with quinoa (½ cup) | 35 | 2‑3 |
| Dinner | Salmon, roasted sweet potato (½ cup), broccoli | 40 | 3‑4 |
| Snack | Apple + 10 almonds | 20 | 1‑2 |
Special Situations
Exercise, illness, and alcohol each throw a curveball. Before a long run, reduce your bolus by 10‑20 % and check glucose before, during, and after. When you’re sick, follow “sick‑day rules”: keep carbs handy, monitor every 2 hours, and never skip insulin—even if you feel fine.
Active Lifestyle
Exercise Improves Insulin Sensitivity
Regular movement is like polishing the hinges on a door—you’ll need less force (insulin) to open it.
Recommended Mix
Aim for 150 minutes of moderate aerobic activity (brisk walking, cycling) plus two strength‑training sessions weekly. This combination boosts glucose uptake for up to 24 hours post‑workout.
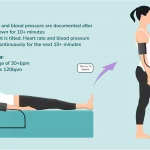
Pre‑ and Post‑Workout Checks
Check glucose 15 minutes before you start. If it’s below 100 mg/dL, snack on 15‑20 g fast carbs. After finishing, re‑check; if it’s high, you might need a small correction bolus.
Stress, Sleep, and Mental Health
Stress releases cortisol, which can nudge glucose upward. Simple mindfulness apps or a 5‑minute breathing exercise can keep those spikes at bay. And never underestimate sleep—poor rest can sabotage insulin sensitivity.
Data Review
Daily Logging
Whether you pen notes in a journal or use an app, capture four data points: time, glucose, insulin, carbs. Over weeks, patterns emerge—maybe you’re consistently high after lunch because of hidden sugars.
Exporting Data for Your Doctor
Most CGMs let you download a CSV file. Bring it to your quarterly appointment; your clinician can spot trends you might miss.
When to Adjust Doses
Look for recurring “dawn phenomenon” (early‑morning highs) or night‑time lows. A common tweak: increase basal by 10 % for dawn highs, or add a small snack before bed for nighttime lows.
Risk Management
Hypoglycemia (Low Blood Sugar)
Early signs include shakiness, sweating, or a sudden urge for sweets. Keep fast‑acting carbs—glucose tablets, juice, or candy—within arm’s reach. If you can’t swallow, a glucagon injection (or nasal spray) is a lifesaver.
Prevention with CGM Alerts
Set low‑glucose alerts at 70 mg/dL. The alarm gives you a heads‑up before you hit the ground.
Hyperglycemia & Ketoacidosis
Persistent highs (>250 mg/dL) can lead to diabetic ketoacidosis (DKA). If you feel nauseous, have fruity breath, or are unusually tired, check glucose, hydrate, and administer a correction bolus. Seek emergency care if you can’t bring levels below 250 mg/dL within an hour.
Long‑Term Complication Screening
Annual eye exams, kidney function tests, and foot checks are non‑negotiable. Keeping A1C under 7 % lowers the risk of these complications dramatically (American Diabetes Society).
Emerging Therapies
Adjunct Medications
Sometimes doctors add metformin, pramlintide, or even low‑dose SGLT‑2 inhibitors to smooth out glucose curves. These aren’t cures—just extra tools for stubborn cases.
Immunotherapy & Beta‑Cell Preservation
Research is racing to stop the autoimmune attack that destroys insulin‑producing cells. Trials using anti‑CD3 antibodies or ATG‑GCSF combos show promise, but they’re still experimental.
Natural Adjuncts—Myth vs. Science
Supplements like vitamin D, omega‑3, or cinnamon are often touted. The evidence is mixed; a 2023 meta‑analysis found only modest glucose benefits from vitamin D when levels were deficient. Always discuss supplements with your care team before adding them.
Conclusion
Treating type 1 diabetes isn’t a one‑size‑fits‑all prescription; it’s a lifelong partnership between you, your body, and your care team. By mastering insulin basics, embracing modern tech, feeding your body with the right carbs, staying active, and keeping an eye on data, you can keep blood‑sugar swings to a minimum and focus on what truly matters—living the life you love.
Take the first step today: schedule a quick review with your diabetes educator, try a CGM demo if you haven’t yet, or simply download the Weekly Treatment Tracker below and start logging. Remember, you’re not alone on this journey—every tip, every adjustment, and every small win adds up to big, lasting control.























Leave a Reply
You must be logged in to post a comment.