Hey there, friend. If you or a loved one are facing colon cancer, the word “complications” can feel like a heavy cloud hanging over everything you hoped for. The good news? Knowing exactly what can happen—and how to spot it early—gives you real power to act, stay safe, and keep hope alive. Below, I’ll walk you through the most common complications, the risks that come with each treatment, and practical steps you can take right now. Let’s dive in together, side‑by‑side.
Why Knowing Complications
First off, why does it matter to learn about complications at all? Because colon cancer isn’t just a single problem—it’s a moving target. The disease itself can cause sudden emergencies, while the colon cancer treatment you choose (surgery, chemo, radiation, targeted therapy) can bring its own set of challenges. Understanding both sides helps you balance the upside of fighting the cancer with the downside of potential side effects, and it lets you and your medical team catch warning signs before they become emergencies.
Complication Overview Guide
In the world of cancer care, “complications” means any unwanted medical event that arises because of the disease or the therapy you receive. They can be acute (show up quickly, often requiring emergency care) or chronic (develop over weeks or months). The good part? Most of these complications are predictable, and with the right monitoring they’re often preventable or treatable.
What Are Complications?
Think of complications as the body’s side‑effects to the battle it’s fighting. A growing tumor can physically block the bowel, erode blood vessels, or even burst through the intestinal wall. Meanwhile, surgery might cause leaks, infections, or scar tissue, and chemo can lead to low blood counts or nerve changes. When you hear doctors talk about “complications,” they’re essentially describing the unintended consequences of both the enemy (the cancer) and the weapons (the treatment).
How Common Are They?
Studies show that roughly 10‑30 % of newly diagnosed colon cancer patients experience an acute complication at some point during their disease course. A 2014 NCBI study examined 1,200 patients and found that bowel obstruction, perforation, and severe bleeding were the three most frequent emergencies (a study).
Key Risk Factors
- Large tumor size or location in the left colon (more likely to block the lumen)
- Advanced stage (III‑IV) where the cancer has already invaded nearby tissues
- Older age or existing health conditions like diabetes or heart disease
- Type of planned colon cancer treatment – aggressive chemo or combined chemo‑radiation raises certain risks
| Stage | Risk of Acute Complication | Typical Complications |
|---|---|---|
| I‑II (early) | ~5 % | Minor bleeding, anemia |
| III (regional spread) | ~15 % | Obstruction, perforation |
| IV (metastatic) | ~30 % | Bleeding, fistulas, severe malnutrition |
Acute Complications Explained
Acute issues pop up quickly, often with dramatic symptoms that demand prompt medical attention. Let’s break down the four biggest emergency‑type complications.
Bowel Obstruction
A tumor can act like a roadblock in your intestine, stopping food and stool from moving forward. Symptoms usually include crampy abdominal pain, swelling, nausea, vomiting, and an inability to pass gas or stool. If you notice a sudden “full” feeling that doesn’t go away, it’s time to call your doctor.
According to Dr. Praveen Kammar’s blog, a 58‑year‑old patient once arrived at the ER wheezing and clutching his abdomen—the tumor had grown large enough to completely block the colon, requiring emergency surgery (according to).
Intestinal Perforation
When a tumor erodes through the full thickness of the bowel wall, it creates a hole. Bowel contents spill into the abdominal cavity, leading to peritonitis—a life‑threatening infection. Signs include sudden, severe abdominal pain, fever, and a rigid “board‑like” abdomen. This is a surgical emergency; mortality can reach 15 % when not treated promptly (a study).
Severe Bleeding / Anemia
Colon cancers often develop ulcerated surfaces that bleed. You might see bright red blood in the stool, dark tarry stools, or feel dizzy from a drop in hemoglobin. A quick blood test can confirm anemia, and endoscopic or angiographic procedures can stop the bleeding. Transfusions are considered when Hb falls below 7‑8 g/dL or if you’re symptomatic.
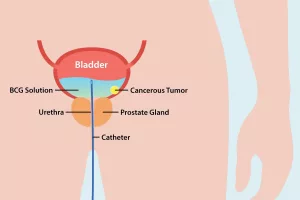
Fistula Formation
A fistula is an abnormal connection between the colon and another organ, most commonly the bladder (colovesical fistula) or the vagina (colo‑vaginal fistula). Symptoms can be puzzling—recurrent urinary tract infections, passage of gas or stool in the urine, or a constant foul odor. These require imaging (CT, MRI) and often surgical repair.
Quick‑Reference Checklist
- Sudden, severe abdominal pain → call emergency services.
- Vomiting, bloating, no stool/gas for 24 hrs → contact your surgeon.
- Black/tarry stools or bright red bleeding → call your oncologist.
- Fever with abdominal tenderness → seek immediate care.
Long-Term Complications Overview
Even after the storm passes, some issues can linger for months or years. These are the “slow‑burn” complications that affect quality of life and sometimes the overall colon cancer prognosis.
Nutritional Deficiencies & Malnutrition
When parts of the colon are removed or when the tumor interferes with absorption, you may lose weight, feel constantly tired, or develop low levels of iron, vitamin B12, or albumin. Regular labs (CBC, ferritin, vitamin levels) and a dietitian’s guidance can keep you nourished. Small, frequent meals rich in protein and healthy fats work wonders.
Strictures & Scarring
After surgery or radiation, scar tissue can tighten the bowel (a stricture), causing intermittent blockage. Symptoms mimic obstruction but are usually less severe. Endoscopic dilation or, in rare cases, a repeat surgery can relieve the narrowing.
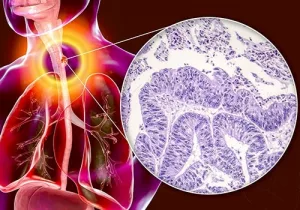
Recurrence & Metastatic Spread
Even after the primary tumor is removed, cancer cells can lurk elsewhere. Ongoing surveillance—regular CT scans, colonoscopies, and carcinoembryonic antigen (CEA) blood tests—helps detect recurrence early, when it’s most treatable. The risk of recurrence is closely linked to the original stage; early‑stage disease (I‑II) has a 5‑year survival over 80 %, while stage IV drops to around 14 % (according to).
Psychosocial Impact
Living with cancer isn’t only a physical battle; the emotional toll can be huge. Anxiety, depression, and what some call “cancer‑related PTSD” affect a sizable number of patients. Joining support groups, talking to a therapist, or even sharing your story with friends (like you’re doing now) can lighten that burden.
Late Treatment‑Related Side Effects
- Radiation enteritis: chronic inflammation of the intestine after radiation, leading to cramping and diarrhea.
- Chemotherapy neuropathy: tingling or numbness in hands and feet, often reversible but sometimes lasting.
- Targeted therapy rash: EGFR inhibitors can cause a red, acne‑like rash on the face and neck.
- Immunotherapy colitis: inflammation of the colon from checkpoint inhibitors, treatable with steroids.
Treatment‑Related Complications
Every treatment option carries its own risk profile. Knowing these helps you weigh benefits against potential harms.
Surgery (Colon Resection) Complications
Removing the cancerous segment (often called a colectomy) is a cornerstone of cure, but it can bring:
- Leaks at the join (anastomotic leak)
- Infection or abscess formation
- Incisional hernia (bulging at the scar site)
- Stricture from scar tissue
- Injury to nearby bladder, ureters, or blood vessels
Stanford Health Care lists these as the most common post‑op concerns (according to), with leaks occurring in about 3‑5 % of cases and hernias in roughly 10 % after laparoscopic surgery.
Open vs. Laparoscopic vs. Robotic
| Approach | Leak Rate | Infection Rate | Avg. Hospital Stay |
|---|---|---|---|
| Open | 5‑7 % | 12‑15 % | 7‑10 days |
| Laparoscopic | 3‑5 % | 8‑10 % | 4‑6 days |
| Robotic | 2‑4 % | 6‑9 % | 4‑5 days |
Chemotherapy‑Related Complications
Chemo attacks rapidly dividing cells, which unfortunately includes healthy bone‑marrow cells. Common side effects include:
- Myelosuppression (low blood counts) → higher infection risk.
- Mucositis (mouth sores) → trouble eating.
- Peripheral neuropathy → tingling in hands/feet.
- Fatigue – the notorious “cancer fatigue” that can linger weeks after cycles end.
Most of these are manageable with growth‑factor injections, dose adjustments, and supportive care.
Radiation Therapy Complications
Radiation targets the tumor and the surrounding tissue. Short‑term side effects are usually limited to skin irritation and diarrhea. Long‑term, however, you might face chronic radiation enteritis, strictures, or, very rarely, a secondary malignancy. Modern techniques (IMRT, proton therapy) dramatically lower these risks.
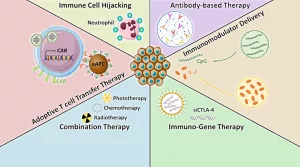
Targeted & Immunotherapy Toxicities
Targeted drugs (like bevacizumab) can cause hypertension, bleeding, or wound‑healing problems. Immune checkpoint inhibitors (pembrolizumab, nivolumab) unleash the immune system and sometimes cause colitis, hepatitis, or thyroid problems. Regular labs and prompt reporting of new symptoms keep these side effects in check.
Balancing Benefits & Risks
Every patient’s situation is unique. A helpful framework is the “benefit‑risk matrix”: score the expected increase in survival or quality of life against the probability and severity of each complication. Collaborate with your oncologist, surgeon, and nutritionist to make the most informed choice.
Detecting Complications Early
Early detection is the secret sauce that turns many complications from life‑threatening to manageable. Here’s a straightforward plan you can start today.
Red‑Flag Symptoms You Should Never Ignore
- Sudden, severe abdominal pain or rigidity.
- Vomiting that won’t stop, especially if you can’t pass gas.
- Black, tarry stools or bright red blood.
- Fever > 38 °C (100.4 °F) with abdominal tenderness.
- Unexplained weight loss > 5 % of body weight in a month.
- New urinary symptoms (painful urination, gas in urine).
Routine Monitoring Plan
Work with your care team to set a schedule:
- Blood work (CBC, electrolytes, liver enzymes) every 2‑4 weeks during chemo.
- CEA levels every 3‑6 months after treatment.
- CT or MRI scans every 6‑12 months depending on stage.
- Colonoscopy 1 year after surgery, then every 3‑5 years.
Multidisciplinary Team Involvement
Don’t try to juggle everything alone. A solid team includes:
- Medical oncologist – oversees chemo, targeted therapy, immunotherapy.
- Colorectal surgeon – handles operative issues and post‑op follow‑up.
- Radiation oncologist – manages radiation plans and side‑effects.
- Nutritionist – addresses malnutrition and dietary adjustments.
- Palliative‑care specialist – focuses on symptom control and quality of life.
- Psychologist or social worker – supports mental health.
Patient‑Reported Outcome Tools
Tools like PRO‑CTCAE let you grade your own symptoms (pain, fatigue, nausea). Sharing these scores with your team has been shown to catch complications earlier and reduce hospitalizations.
Takeaway
Colon cancer complications are a reality, but they’re not a mystery. By understanding the common acute emergencies—obstruction, perforation, bleeding, and fistulas—and the longer‑term challenges like malnutrition, strictures, and treatment side effects, you can stay one step ahead. Pair that knowledge with a clear monitoring plan, a supportive multidisciplinary team, and the willingness to speak up when something feels off, and you create a powerful safety net for yourself or a loved one.
Remember, you’re not alone in this journey. Whether you’re questioning a new symptom, debating a treatment option, or just need a listening ear, feel free to share your thoughts in the comments below. Your story might be the very thing that helps someone else find their own path through the maze of colon cancer. Stay hopeful, stay informed, and keep moving forward.



















Leave a Reply
You must be logged in to post a comment.