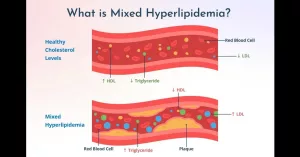
Imagine your bloodstream as a busy highway. When traffic is smooth, everything runs nicely. But if several lanes are clogged at once—high LDL, high triglycerides, and low “good” HDL—you’ve got a perfect storm that can bring a heart‑attack‑inducing traffic jam. That’s basically what mixed hyperlipidemia does. In the next few minutes we’ll break down what it means, why it matters, and how you can steer your health back onto an open road.
Why It Matters
Quick answers for your top questions
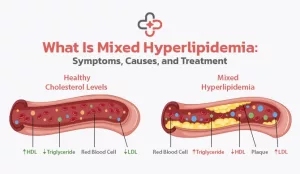
What is mixed hyperlipidemia? It’s a lipid disorder where low‑density lipoprotein cholesterol (LDL‑C) and triglycerides (TG) are both elevated while high‑density lipoprotein cholesterol (HDL‑C) often drops. The combination multiplies cardiovascular risk far beyond a single‑lipid abnormality.
How dangerous is it? If left untreated, the risk of heart attack, stroke, and peripheral artery disease can be two to three times higher than in people with only one abnormal lipid type.
Can I control it? Absolutely. Lifestyle tweaks plus, when needed, medication can bring numbers back into a safe range and dramatically cut your risk.
Understanding Mixed Hyperlipidemia
What “mixed” really means
The word “mixed” signals that more than one lipid class is out of balance. A typical lab picture looks like this:
- LDL‑C: 130 mg/dL + (High)
- Triglycerides: 250 mg/dL + (High)
- HDL‑C: 35 mg/dL – (Low)
This triad pushes plaque formation faster than any single abnormality. You’ll often see the term “familial combined hyperlipidemia” (FCHL) used interchangeably—especially when genetics are a big part of the story.
How doctors diagnose it
Diagnosis starts with a fasting lipid panel. If the numbers match the mixed pattern, doctors may order an ICD‑10 code (E78.01) to document the condition. Some specialists also check apolipoprotein B, because it’s a reliable marker of elevated LDL particles (ScienceDirect study).
Who’s most likely to get it?
If one of your parents carries the gene, you have roughly a 50 % chance of inheriting the predisposition. Even without a family history, the condition shows up often in people with metabolic syndrome—think obesity, type‑2 diabetes, high blood pressure, and excess abdominal fat (BMJ 2011).
Symptoms & Risks
Does it hurt?
Most people feel fine. That’s why screening matters. When symptoms do appear, they’re usually clues rather than the disease itself:
- Xanthomas: yellowish fatty bumps on elbows, knees, or tendons.
- Arcus corneae: a whitish ring around the eye.
- Chest discomfort or leg cramping during exercise—signs that arteries are narrowing.
What could go wrong?
The biggest danger is accelerated atherosclerosis. Plaque builds up faster because LDL‑C deposits cholesterol while high TG fuels inflammation. Over time this can lead to:
- Coronary artery disease and heart attacks.
- Ischemic strokes.
- Peripheral vascular disease (painful legs, ulcers).
Untreated mixed hyperlipidemia can shave years off life expectancy. A recent review notes that aggressive treatment can bring cardiovascular risk back to near‑average levels (HealthGrades).
Root Causes
Genetics – the inherited part
FCHL is polygenic—multiple genes tilt the balance toward high LDL and TG. Elevated apolipoprotein B is a hallmark (ScienceDirect).
Lifestyle – the modifiable part
Even a strong genetic background can be worsened by everyday choices:
- Diet: Lots of saturated fat, refined carbs, and sugary drinks spike triglycerides.
- Sedentary habits: Lack of exercise lowers HDL‑C and raises TG.
- Alcohol: Over‑drinking pushes triglycerides sky‑high.
- Weight gain: Extra belly fat fuels insulin resistance, which fuels mixed lipids.
Think of it like a dimmer switch—your genes set the maximum brightness, but your lifestyle decides how low you can turn it.
Treatment Options
First line: Lifestyle changes
Before you reach for a pill, try these proven moves:
- Heart‑healthy eating: Mediterranean‑style meals rich in olive oil, nuts, fish, whole grains, and plenty of veggies. Aim for at least 30 g of soluble fiber a day (oats, beans, apples).
- Move more: 150 minutes of moderate aerobic activity (brisk walking, cycling) plus two strength sessions weekly can lift HDL‑C by 5‑10 %.
- Weight loss: Shedding just 5‑10 % of body weight can drop triglycerides by up to 30 %.
- Alcohol moderation: No more than one drink per day for women, two for men.
When medication is needed
If labs stay stubborn after three months of lifestyle work, medication steps in.
- Statins: The go‑to for lowering LDL‑C. Studies show they also modestly improve HDL‑C and reduce cardiovascular events (Ballantyne 2001).
- Fibrates (e.g., fenofibrate): Best for high triglycerides and can raise HDL‑C.
- Omega‑3 EPA/DHA: Prescription‑strength fish oil lowers TG dramatically with few side effects.
- Combination therapy: Statin + fibrate or statin + niacin works for some, but watch for liver enzyme elevations and muscle aches.
Choosing the right path
Here’s a simple decision flow you can discuss with your doctor:
- LDL‑C > 100 mg/dL? → Start a statin.
- Triglycerides > 200 mg/dL after 3 months? → Add a fibrate or omega‑3.
- HDL‑C < 40 mg/dL? → Emphasize exercise, consider niacin if tolerated.
Living With Mixed Hyperlipidemia
Daily nutrition hacks
Swap butter for avocado or olive oil, trade soda for sparkling water with a splash of citrus, and sprinkle chia or flaxseed on oatmeal for extra omega‑3s. Small swaps add up quickly.
Exercise ideas that stick
Pick activities you enjoy—dance classes, hiking with friends, or a weekend bike ride. Consistency beats intensity; even a 30‑minute walk after dinner counts.
Monitoring your progress
Schedule a fasting lipid panel after you start any new medication or lifestyle regime (usually 6‑8 weeks). Keep a simple spreadsheet: date, LDL‑C, TG, HDL‑C, weight, and notes about diet or exercise. Seeing numbers improve is incredibly motivating.
Mind‑body balance
Stress hormones can raise triglycerides, so take time for relaxation—whether it’s yoga, deep‑breathing, or a good book. Remember, caring for your heart is a marathon, not a sprint.
Bottom Line – Take Action Today
Mixed hyperlipidemia mixes high LDL‑C, high triglycerides, and often low HDL‑C into a dangerous cocktail. The good news? You have the power to turn the tide. Start with a friendly chat with your doctor about a lipid panel—if you’ve got a family history, don’t wait (What is mixed hyperlipidemia).
From there, embrace a heart‑smart diet, move daily, and keep an eye on your numbers. If lifestyle alone isn’t enough, modern medication—statins, fibrates, omega‑3s—can safely bring your lipids back into range. And remember, treating mixed hyperlipidemia isn’t just about numbers; it’s about preserving the moments you love—family gatherings, hikes, and everything in between.
Curious about how long you might live with this condition? Check out our guide on mixed hyperlipidemia life expectancy for a realistic outlook and hopeful strategies.
We’ve covered the “what,” “why,” and “how.” Now it’s your turn. What steps will you take today to protect your heart? If you have questions, feel free to reach out to a trusted healthcare professional—your future self will thank you.






















Leave a Reply
You must be logged in to post a comment.