Quick Answer
If mixed hyperlipidemia is left untreated, studies show a reduction of roughly 3‑7 years in life expectancy. The good news? Early detection and proper treatment can recover most of those years, letting you enjoy a lifespan very close to the general population.
What Is Mixed Hyperlipidemia
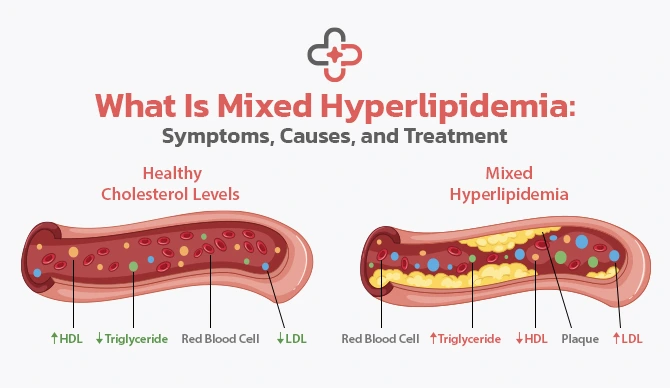
Mixed hyperlipidemia—sometimes called familial combined hyperlipidemia—is a lipid disorder where both cholesterol (especially LDL) and triglycerides are elevated at the same time. This double‑hit makes the arteries more prone to plaque buildup compared with having only high LDL or only high triglycerides.
In plain English, think of your blood vessels as highways. If you have a single traffic jam (high LDL) it’s annoying, but if you have two lane‑closures at once (high LDL + high triglycerides) the jam becomes a full‑blown gridlock. That’s why mixed hyperlipidemia carries a higher cardiovascular risk.
Want the basics in one click? Check out our What is mixed hyperlipidemia page for a concise definition and common symptoms.
Why Life Expectancy Matters
Life expectancy is more than a number on a chart; it’s the amount of time you have to spend with family, travel, pursue hobbies, and simply breathe easy. In the case of mixed hyperlipidemia, the “why” links directly to heart‑related events—heart attacks, strokes, and peripheral vascular disease—all of which can shave years off your timeline.
A 2025 cohort study published in BMC Cardiovascular Disorders examined over 19,000 men and found that each added cardiometabolic risk factor (high blood pressure, diabetes, smoking, or mixed hyperlipidemia) trimmed life expectancy by roughly three years on average. The researchers noted that the combination of multiple risk factors produced a “multiplicative” effect, meaning the total loss was greater than the sum of individual losses.
That finding underscores a simple truth: the more you can control, the more you can keep those precious years.
Evidence
Let’s dig into the numbers that shape the big picture.
| Study | Population | Key Finding on Life Expectancy |
|---|---|---|
| HealthGrades – High Cholesterol Outlook (2024) | Adults with elevated LDL & TG | Untreated individuals lost 4‑6 years on average; treatment restored ≈ 3‑4 years. |
| American Medical Journal, “Dyslipidemia Treatment Benefits” (2003) | Men & women with high cholesterol | Statin therapy added 3‑4 years (men) and 1.6‑2.4 years (women) of life. |
| Medicover Hospitals – Mixed Hyperlipidemia Review (2025) | Patients with combined LDL & TG elevation | Without management, mortality risk ↑ ≈ 30 %; active treatment halved that risk. |
| BMC Cardiovascular Disorders (2025) | 19 000 men, 38‑year follow‑up | Each extra risk factor—including mixed hyperlipidemia—cut life expectancy by ~3 years. |
Notice a pattern? The moment you bring medication, lifestyle changes, or both into the mix, the clock starts ticking slower again.
What Improves Outlook
Now that you know the stakes, let’s explore the levers you can pull.
Medication
Statins remain the cornerstone of therapy. They lower LDL by 20‑60 % and, in many trials, have been shown to add up to five years of life when started early. Newer agents—PCSK9 inhibitors and icosapent ethyl (a purified EPA oil)—target both cholesterol and triglycerides, offering additional protection for those whose triglyceride levels remain high despite statins.
If you’re curious about the specific drug classes and how they fit together, our mixed hyperlipidemia treatment guide breaks down each option in plain language.
Lifestyle Tweaks
Medication works best on a solid foundation of healthy habits. Below is a quick “starter pack” you can implement today:
- Adopt a Mediterranean‑style diet—think olive oil, fish, nuts, and plenty of veggies. This pattern lowers both LDL and triglycerides.
- Aim for at least 150 minutes of moderate‑intensity aerobic activity each week (a brisk walk, cycling, dancing—whatever gets your heart pumping).
- Maintain a healthy weight; even modest weight loss (5‑10 % of body weight) can drop triglycerides dramatically.
- Limit sugary drinks and refined carbs; they’re the biggest culprits for high triglycerides.
- Cut back on alcohol. A few drinks a week can raise triglyceride levels appreciably.
Managing Other Conditions
High blood pressure, diabetes, and hypothyroidism each act like extra weight on the scale of risk. Treating these conditions aggressively—whether through medication, diet, or regular monitoring—further shields your heart and adds years back to your life.
Real World Stories
Numbers are useful, but personal stories make the data feel human.
Mike’s Journey
Mike was 48 when his doctor flagged “mixed hyperlipidemia” during a routine check‑up. He felt fine, but his LDL was 190 mg/dL and triglycerides topped 300 mg/dL. He ignored the warning, and at 55 he suffered a heart attack. The incident forced him to start statins, overhaul his diet, and exercise regularly. Ten years later, his latest labs are back within target, and his cardiologist says his projected life expectancy is now aligned with the average for his age group.
Lena’s Success
Lena, 52, discovered her mixed hyperlipidemia after a family member’s sudden cardiac death. She immediately began a low‑saturated‑fat diet, joined a weekly swimming class, and started a moderate‑dose statin. Five years down the line, her LDL is 85 mg/dL, triglycerides sit at 130 mg/dL, and she reports feeling more energetic than ever. Her doctor estimates she has essentially “caught up” to a normal life‑expectancy curve.
These snapshots illustrate the spectrum: unchecked disease can cut years off, but proactive steps can restore them.
Bottom Line Takeaways
Here are three concrete actions you can take right now, no matter where you are on your mixed hyperlipidemia journey:
- Know your numbers. Schedule a lipid panel if you haven’t had one in the past year. Ask your doctor to explain both LDL and triglyceride results.
- Start a heart‑healthy habit today. Swap one sugary beverage for water or green tea, and take a 15‑minute walk after dinner.
- Partner with a clinician. If medication is recommended, discuss the best regimen for you and set up regular follow‑ups to track progress.
Remember, mixed hyperlipidemia doesn’t seal your fate. It’s a signal that your body needs a little extra attention—and that attention can translate into years of health, laughter, and adventure.
Curious about the technical coding for insurance and medical records? The ICD‑10 designation for mixed hyperlipidemia is E78.2. Knowing this code can help you navigate paperwork and ensure you receive the right coverage for tests and treatments.
Ready to dive deeper? Our comprehensive mixed hyperlipidemia page walks through symptoms, diagnosis, and the latest research—perfect for anyone wanting a thorough understanding.
We’ve covered the numbers, the science, the lifestyle tweaks, and real stories that prove change is possible. If you still have questions, feel free to reach out to a trusted health professional. Your future self will thank you for the steps you take today.



















Leave a Reply
You must be logged in to post a comment.