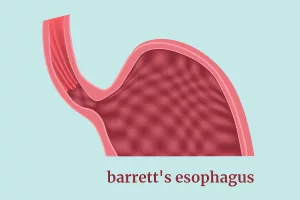
Most people don’t realize that you can check for Barrett’s esophagus, esophageal cancer, or hidden gastrointestinal bleeding without having to lie on a table while a long, flexible tube is shoved down your throat. If you’ve ever felt a pang of anxiety at the thought of an endoscopy, you’re not alone. The good news is that a whole suite of endoscopy alternatives now exists, offering comparable diagnostic power with far less discomfort.
In the next few minutes we’ll walk through the most promising options, explain when each one shines, and help you decide what might fit your lifestyle and health needs. Think of this as a friendly coffee‑table chat with a gastro‑enthusiast who’s done the homework, spoken to specialists, and tried a few of these tools firsthand.
Criteria for Good Alternatives
Diagnostic accuracy matters
Any test that claims to replace a traditional endoscopy must first prove it can see what doctors need to see. Studies consistently compare sensitivity (how well the test finds disease) and specificity (how well it rules out disease) against the gold‑standard endoscopy. For most screening purposes, a sensitivity above 85 % and a specificity above 80 % are considered acceptable.
Patient comfort is non‑negotiable
We’re talking about procedures people can tolerate without heavy sedation, gag reflexes, or long recovery times. The less you have to “brace yourself,” the more likely you’ll actually follow through and get screened on schedule.
Cost and accessibility
Even the most brilliant technology is useless if it’s locked behind a paywall that only a handful of clinics can afford. Look for FDA‑cleared or CE‑marked devices that are reimbursable under typical health plans.
Safety profile
Every technique carries some risk—capsule retention, minor nasal irritation, or rare allergic reactions. The key is to understand the frequency of complications and whether they’re manageable.
Expert insight
According to a 2024 ASGE guideline, “the choice of an endoscopy alternative should be guided by patient preference, clinical indication, and the availability of expertise to interpret the results” a 2024 guideline. In practice, this means doctors weigh the pros and cons with you, not the other way around.
Transnasal Esophagoscopy
How it works
Transnasal esophagoscopy (TNE) swaps the traditional mouth‑entry route for a thin, flexible tube that slides gently through the nostril. Because the scope is slender—about the width of a pencil—and usually doesn’t require sedation, most patients stay fully awake and report minimal discomfort.
Who benefits most?
If you’re being monitored for Barrett’s esophagus, have mild dysphagia, or need an early look for esophageal cancer, TNE is a perfect match. A 2024 study by Lim et al. found that over 90 % of patients tolerated the procedure without any need for sedation, and physicians could obtain high‑quality images of the upper esophagus.
Pros & Cons
| Pros | Cons |
|---|---|
|
|
Capsule‑Based Technologies
Pill‑on‑a‑Thread Test
The Pill‑on‑a‑Thread (also called the Esophageal String Test) is a clever little device: a thin, flexible thread attached to a tiny gelatin capsule is swallowed. After a few minutes, the capsule dissolves, releasing a sponge that collects cells from the esophagus. The thread is then pulled back out, bringing the collected sample for lab analysis.
Because it’s essentially a “sponge‑on‑a‑string,” there’s no need for an endoscope at all. It’s especially useful for patients who need regular monitoring of Barrett’s or who cannot tolerate any form of scope.
Read more about how this test works here.
Capsule Sponge Test
The capsule sponge test takes the concept a step further. You swallow a tiny capsule that contains a compressed sponge. Once it reaches the esophagus, the capsule opens, allowing the sponge to expand and brush against the lining, gathering cells for a pathology review. FDA‑cleared for Barrett’s screening, it’s been praised for its comfort and reliability.
Curious about the details? Dive into our full guide here.
Video Capsule Endoscopy (VCE)
When the question is “Where is that hidden bleed in my small intestine?” the answer often lies in a pill‑sized camera that travels the entire GI tract while streaming thousands of images to a wearable recorder. The device—often branded PillCam™—doesn’t need sedation, wires, or a hospital stay. After about eight hours, the capsule exits naturally, and the images are uploaded for a gastroenterologist’s review.
Performance snapshot
| Indication | Detection Rate | Key Limitation |
|---|---|---|
| Obscure GI bleeding | ≈85 % sensitivity | Capsule retention ~1 % (higher with strictures) |
| Crohn’s disease assessment | ≈78 % sensitivity | Cannot obtain biopsies |
| Small‑bowel tumors | ≈70 % sensitivity | Limited depth perception |
Advanced Optical Options
Endomicroscopy
Endomicroscopy slides a microscopic probe through the nose or a very thin channel, giving a real‑time, cellular‑level view of the mucosa. It’s like having a microscope on a nano‑scale, which can spot dysplasia in Barrett’s before it becomes visible to the naked eye. While still mostly in specialized centers, it represents a future where “see‑and‑treat” could happen without a full‑blown endoscopy.
Cell‑Collection Devices
Beyond the pill‑on‑a‑thread and capsule sponge, newer “sponge‑balloon” and “string‑balloon” devices are being piloted for less invasive screening of the upper GI tract. They combine gentle suction with brush‑like sampling, delivering a high‑quality specimen while the patient remains fully conscious.
When Endoscopy Still Needed
Therapeutic interventions
There are moments when a doctor needs to not just look but act—remove a polyp, cauterize a bleeding vessel, or inject medication directly into tissue. Traditional upper or lower endoscopy is still the workhorse for those therapeutic tasks. If your clinician suspects high‑grade dysplasia, early cancer requiring resection, or needs to place a stent, a conventional scope will be part of the plan.
Biopsy‑driven diagnoses
While many alternatives can collect cells, they rarely provide the depth and architecture a full biopsy offers. For definitive cancer staging or when the microscopic pattern matters (e.g., eosinophilic esophagitis), a standard endoscopic biopsy remains gold‑standard.
Balancing Benefits & Risks
Quick decision checklist
| Situation | Best Alternative | Key Benefit | Main Risk | Talk To Your Doctor About… |
|---|---|---|---|---|
| Routine Barrett’s surveillance | Transnasal ES | Minimal discomfort, office‑based | Rare nasal irritation | Availability & insurance coverage |
| Obscure GI bleeding | Video Capsule Endoscopy | Full small‑bowel view without sedation | Capsule retention (≈1 %) | History of strictures or Crohn’s |
| Frequent monitoring (e.g., EoE) | Pill‑on‑a‑Thread / Capsule Sponge | Cell collection without scope | Potential inadequate sample if not performed correctly | Training of the staff |
| Need for therapeutic action | Traditional endoscopy | Biopsy, polyp removal, laser | Requires sedation, gag reflex | Pre‑procedure preparation |
Future Directions
Robotic colonoscopy & AI
Emerging robotic platforms promise smoother navigation and AI‑driven lesion detection, potentially lowering miss rates and patient discomfort. Early trials suggest a 15 % reduction in procedure time and a higher detection rate for flat lesions.
Smart capsules with biopsy capability
Researchers are prototyping capsules that can fire micro‑needles or release a small amount of suction to grab tissue. Though still in clinical trials, these “biopsy‑capsules” could one day make the invasive scope truly optional.
Preparation & Expectations
Before the test
- Fast for 8–12 hours (water allowed only if instructed).
- Discuss all medications—especially iron supplements, anti‑platelets, or NSAIDs—with your doctor.
- Tell the team if you have a pacemaker, a history of strictures, or swallowing difficulties.
During the procedure
Most alternatives are performed while you sit in a waiting‑room chair. You’ll wear a small recorder on a belt (for video capsules) or simply hold a thin nasal scope. The entire process usually lasts 10–30 minutes, and you can usually resume normal activity immediately afterward.
Afterwards
Results may take a few days to a week, depending on the test. Your gastroenterologist will discuss the images, any findings, and the next steps. If a capsule was used, you’ll be asked to confirm that it passed—most people notice it in their stool within 24–48 hours.
Conclusion
Modern gastroenterology has moved far beyond the “big tube down the throat” stereotype. Whether you need surveillance for Barrett’s esophagus, a check for hidden bleeding, or a gentle way to collect esophageal cells, a reliable endoscopy alternative is likely waiting at your nearest clinic. While traditional endoscopy still holds a vital therapeutic role, the less‑invasive options—transnasal esophagoscopy, pill‑on‑a‑thread, capsule sponge, and video capsule endoscopy—offer comparable diagnostic power with far less discomfort and quicker recovery.
Talk openly with your doctor about your preferences, medical history, and the availability of these technologies. With the right information, you can choose a path that feels comfortable, cost‑effective, and clinically sound. Your gut health deserves attention, and now you have the tools to get screened without the dread.




















Leave a Reply
You must be logged in to post a comment.