Hey there, friend. If you’ve ever stared at the scale and wondered why, despite all the binge‑purge cycles, the numbers are creeping up, you’re not alone. The short answer? The body’s biology, hidden calories, and the way we think about weight can all turn the “weight‑loss” plan upside‑down. In this post I’ll walk you through why weight gain can be a part of bulimia, bust some myths, and share concrete steps you can start using today to feel safer about your weight while you get help.
Let’s dive in together—no fluff, just honest, practical info that you can actually use. Grab a cup of tea, and let’s chat.
Why Weight Gain Happens
Hidden calories in the binge‑purge cycle
When you binge, you might think you’re “eating a lot” but the truth is many people underestimate how many calories they actually consume. A typical binge can easily add 1,000–2,000 calories, and purging (whether it’s vomiting, laxatives, or excessive exercise) only removes a fraction of those calories. According to a study from Drexel University, most women with bulimia actually regain weight while they’re still purging. The body’s digestive system simply can’t “undo” the energy you’ve taken in.
The math in plain English
Imagine you’re eating a slice of pizza (≈ 300 kcal). You binge on 3 slices, that’s 900 kcal. Even if you purge once, you might only discard about 10‑15 % of those calories. The rest becomes stored energy, often as fat.
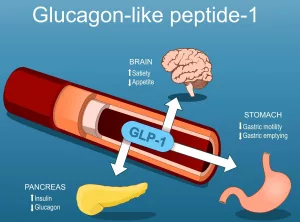
Metabolic & hormonal shifts
Our bodies are smarter than we give them credit for. When you frequently binge and then purge, you confuse the hunger hormones—especially leptin, the “I’m full” signal. Low leptin levels make you feel hungrier, prompting you to eat more. This is why many people notice a sudden surge in appetite after a period of restriction.
Water and carb retention
When you finally start eating regular carbs again, your body restores glycogen stores. Glycogen binds to water—about 3 grams of water per gram of glycogen—so you might see a quick 2–3 kg jump on the scale. That’s mostly water, not fat, but it can feel scary.
Weight‑suppression vs. weight‑stable bodies
“Weight‑suppression” is a term researchers use to describe the gap between your highest adult weight and your current weight. For example, if you once weighed 90 kg and now weigh 75 kg, you’re 15 kg weight‑suppressed. The body often reacts by increasing hunger hormones and decreasing satiety hormones, pushing you toward weight gain.
Why the body “rebounds”
One theory suggests the brain senses a “deficit” and activates mechanisms to restore what it perceives as “normal” weight. Another theory points to emotional coping—when you fear returning to your highest weight, you may engage in stricter dieting, which fuels more binge episodes. Both routes can end in weight gain.
Common Bulimia Myths
Myth: Bulimia always makes you skinny
Reality check: In a large survey, 59‑71 % of women with bulimia hit their highest-ever weight after the disorder started. It’s not just “thin people” who struggle; many experience substantial weight fluctuations.
Myth: Stopping purging leads to instant weight loss
When you stop purging, your body begins to heal. That means re‑hydrating, refilling glycogen, and normalizing hormone levels—all of which can cause a temporary rise on the scale before things level out.
Myth: Gaining weight means treatment failed
On the contrary, gaining weight can signal that your body is finally receiving the nutrition it needs. In cognitive‑behavioral therapy (CBT) programs, the first goal is to stop purging and establish regular eating. When you stick to three meals and two to three snacks a day, weight often stabilizes—sometimes increasing slightly as you recover.
Binge‑Purge Cycle Overview
Typical binge triggers
Stress, diet fatigue, and even seemingly harmless “cheat meals” can ignite a binge. Media messages that glorify thinness or restrict food can also set the stage.
Purging methods & calorie recovery limits
| Method | Estimated Calorie Removal | Effectiveness |
|---|---|---|
| Self‑induced vomiting | ~10‑15 % of binge calories | Harsh on teeth, throat, electrolytes |
| Laxatives | ~5‑10 % (mostly water loss) | Can cause dehydration, electrolyte imbalance |
| Diuretics | ~5‑10 % (water only) | Risk of kidney issues |
| Excessive exercise | Variable, often <10 % of calories | Increases injury risk, stress hormones |
Frequency & severity metrics
Clinical guidelines say a diagnosis of bulimia requires binge‑purge episodes at least once a week for three months. The more frequent the cycle, the higher the risk for rapid weight fluctuations and medical complications.
Map Your Weight History
Calculate your weight‑suppression
Use this simple formula: Highest adult weight – current weight = weight‑suppression. Write it down in a notebook or a phone app. Knowing this number helps you and your therapist understand the biological pressure your body is under.
Tools & trackers
Several free apps let you log meals, binge episodes, and purges. Pair that with a mood tracker—many people notice that certain feelings (loneliness, anxiety) precede binge episodes.
When trends signal risk
Watch for any of these patterns:
- Gaining > 2 kg (≈ 4‑5 lb) in two weeks without a clear reason.
- Steady rise after three months of therapy—might mean your body is finally getting the calories it needs.
- Sudden drop after a period of “controlled” eating—could indicate hidden restriction.
Evidence‑Based Treatment
Cognitive‑behavioral therapy (CBT)
CBT is the gold‑standard for bulimia. It’s broken into three phases: first, stop purging; second, establish regular eating; third, build relapse‑prevention skills. The therapy at Eating Disorder Therapy LA emphasizes three meals plus two to three snacks daily—this structure helps keep blood sugar stable and reduces binge urges.
Nutrition counseling & structured meal plans
Working with a registered dietitian can demystify “what’s a healthy portion?” Rather than counting calories obsessively, you’ll learn to include a balance of protein, healthy fats, and carbs. A sample day might look like:
- Breakfast: Greek yogurt + berries + a sprinkle of granola.
- Snack: Apple slices with almond butter.
- Lunch: Quinoa salad with chickpeas, veggies, and olive‑oil dressing.
- Snack: Whole‑grain crackers + hummus.
- Dinner: Grilled salmon, roasted sweet potatoes, steamed broccoli.
Medical monitoring
Regular blood work checks electrolytes, kidney function, and thyroid health. Dental visits are crucial because repeated vomiting erodes enamel. If you experience persistent vomiting, a psychiatrist may prescribe an SSRI (like fluoxetine) to help curb binge urges.
Complementary approaches
Mindfulness, intuitive eating, and Health at Every Size® (HAES®) principles can shift the focus from weight to well‑being. WithinHealth highlights that gentle movement—yoga or walking—helps regulate mood without the pressure of “burning calories.”
Practical Weight Management
Build a steady‑eating routine
Choose snacks you genuinely enjoy—no “cheat” label required. Think of them as fuel, not a loophole. Some go‑to options are:
- Banana with peanut butter.
- Whole‑grain toast topped with avocado.
- Trail mix (nuts, seeds, a few dark‑chocolate chips).
Hydration & electrolyte balance
Water is your best friend, but if you’ve been using diuretics or laxatives, you might need an electrolyte drink (e.g., a pinch of salt in water with a splash of orange juice). Avoid “water pills”—they don’t replace lost minerals.
Gentle movement instead of compulsive exercise
Swap the “I have to burn 1,000 calories” mentality for a “I’m moving because my body feels good.” A 30‑minute walk in nature, a beginner’s yoga class, or a light bike ride can improve mood without triggering binge urges.
Self‑compassion scripts
When anxiety spikes, try silently saying:
“I’m safe. My body is healing. I deserve nourishment.”
Repeating a kind phrase can interrupt the cycle of self‑criticism that fuels binge‑purge behavior.
Day‑in‑the‑life checklist
| Time | Action | Check |
|---|---|---|
| 7 am | Breakfast – protein + carb | ✅ |
| 10 am | Snack – fruit + nut butter | ✅ |
| 12 pm | Lunch – balanced plate | ✅ |
| 3 pm | Snack – yogurt or cheese | ✅ |
| 6 pm | Dinner – lean protein + veg | ✅ |
| Evening | Gentle walk or stretch | ✅ |
When to Seek Professional Help
Red‑flag signs
If you notice any of these, reach out ASAP:
- Vomiting more than 5 times a week.
- Dental erosion, swollen gums, or persistent sore throat.
- Dizziness, fainting, or irregular heartbeats.
- Missing periods for more than three months.
- Severe anxiety, depression, or thoughts of self‑harm.
Choosing a qualified therapist
Look for a licensed psychologist, psychiatrist, or eating‑disorder specialist who lists “CBT for bulimia” among their services. Many clinicians hold certifications from the International Association of Eating Disorder Professionals (IAEDP).
Levels of care
Depending on severity, you might start with outpatient therapy, then step up to intensive outpatient or a partial‑hospitalization program. Eating Disorder Hope notes that early intervention dramatically reduces the chance of relapse.
Conclusion
Weight gain in bulimia can feel confusing, scary, and even like a setback—but it’s often a natural part of the body’s effort to find balance. Understanding the hidden calories, hormonal shifts, and weight‑suppression dynamics demystifies why the scale behaves the way it does. More importantly, recognizing that gaining weight can be a sign of healing, not failure, opens the door to compassionate, evidence‑based treatment.
If any of what you read resonates with you, please consider reaching out to a qualified therapist or a medical professional. You deserve help that honors both your mind and your body. Remember, you’re not alone on this path—there are people ready to listen, support, and guide you toward a healthier, more peaceful relationship with food and yourself.
























Leave a Reply
You must be logged in to post a comment.