Most people don’t realize that dropping just one percentage point in HbA1c can cut the risk of eye, kidney and heart complications by roughly 35 % 【source 1】. If you’re reading this, you probably want that risk‑lowering magic for yourself or someone you care about. Good news: you don’t need a miracle drug or a radical surgery. A blend of everyday habits, smart medication choices and a dash of perseverance can move the needle on your HbA1c dramatically. Grab a cup of tea, get comfy, and let’s walk through the exact steps you can start using right now.
Why HbA1c Matters
First, a quick refresher. HbA1c (also called A1c) is a blood test that shows your average glucose level over the past two‑to‑three months. Think of it as the “report card” for how well your body is handling sugar. About half of the result reflects the most recent 30 days, so recent changes you make can show up faster than you might expect 【Diabetes Educators Calgary, 2022】.
Target ranges differ a little based on age, pregnancy status and other health factors, but for most adults the sweet spot is below 7 %. The American Diabetes Association recommends staying there because every 1 % drop translates into a substantial cut in micro‑vascular complications – retinopathy, nephropathy, neuropathy – and even big‑picture events like heart attacks and strokes.
Lifestyle Changes
When we talk “lifestyle,” we’re not talking a once‑off diet fad. We’re talking sustainable habits that become part of your daily rhythm. Below are the proven pillars that consistently shave numbers off the A1c scale.
1. Low‑Carb, High‑Fiber Eating
Carbohydrates are the main source of blood glucose spikes. By dialing them down and replacing refined carbs with fiber‑rich veggies, nuts and seeds, you blunt those spikes and let your pancreas breathe. A real‑world example is JB, a 55‑year‑old from Abuja, Nigeria. He ate a 1500‑kcal plan (≈150 g carbs, 75 g protein, 50 g fat) and saw his HbA1c plummet from 12.1 % to 5.3 % in just three months 【JB case study】.
If you’ve never tried counting carbs, start simple: aim for under 150 g per day and keep a food journal for a week. You’ll be surprised how quickly the pattern emerges.
For a deeper dive on carbohydrate management, check out our guide on type 2 diabetes nutrition.
2. Move Your Body Regularly
Exercise isn’t just about burning calories; it directly improves insulin sensitivity. Even a modest 150 minutes of brisk walking or 75 minutes of vigorous activity each week can shave 0.5–1 % off your HbA1c. If you’re pressed for time, break it up: three 10‑minute walks after meals work wonders.
Strength training is another secret weapon. Building muscle gives your cells more “real estate” for glucose uptake, which means lower blood sugar without extra medication.
3. Sleep, Stress & Meal Timing
Sleep deprivation spikes cortisol, the stress hormone that encourages the liver to dump glucose into the bloodstream. Aim for 7–9 hours of quality sleep, and try to avoid heavy meals after 8 p.m. (there’s anecdotal evidence that late‑night eating spikes overnight glucose).
Stress management tools like mindfulness apps, breathing exercises, or simply a hobby you love can also keep your sugar levels steadier. Remember, a calm mind is a healthier body.
4. Weight Management
Losing even 5 % of body weight can translate into a 0.5 % drop in HbA1c. It’s not about crash diets; it’s about creating a modest calorie deficit (200–300 kcal per day) and sticking with it. Pair this with the low‑carb approach above, and the weight loss often follows naturally.
Medication Options
Lifestyle is the foundation, but many people need a medication boost to hit their targets faster or when blood sugar is very high. Below is a quick guide to the most common classes, plus a few newer options that many patients overlook.
First‑Line Oral Agents
Metformin remains the go‑to drug. It lowers HbA1c by about 0.6–1 % and has the added benefit of modest weight loss. If you’re new to diabetes meds, this will likely be your starting point.
Sulfonylureas (e.g., glipizide) can add another 0.5 % reduction, but they carry a higher risk of hypoglycemia, especially if you skip meals.
Basal and Weekly Insulin
When HbA1c climbs above 9 %, basal insulin often becomes necessary. Insulin glargine provides a steady background level and can drop HbA1c by 1–2 %.
For those who dread daily injections, weekly insulin (e.g., insulin efsitora) offers a once‑a‑week routine with comparable efficacy. The convenience factor can improve adherence, especially for busy folks.
SGLT2‑Inhibitors vs. DPP‑4 Inhibitors
A consensus review of over 200 studies showed that SGLT2 inhibitors edge out DPP‑4 inhibitors by a modest 0.1–0.2 % when added to metformin 【Consensus 2024】. They also help with weight loss and cardiovascular protection, making them a solid second‑line choice for many.
GLP‑1 Agonists
GLP‑1 drugs are like a two‑for‑one deal: they can lower HbA1c by 0.8–1.5 % and often lead to weight loss. A clinical resource from the Association of British Clinical Diabetologists notes the dual benefit on glucose and weight according to their data.
Risk‑Benefit Comparison
| Therapy | Avg HbA1c ↓ | Typical Side‑Effects | When to Use |
|---|---|---|---|
| Metformin | 0.6–1.0 % | GI upset | First‑line for most |
| Basal insulin | 1.0–2.0 % | Hypoglycemia, weight gain | HbA1c > 9 % |
| SGLT2‑i | 0.3–0.5 % | UTIs, ketoacidosis | CKD or CVD risk |
| GLP‑1 agonist | 0.8–1.5 % | Nausea, pancreatitis | Need weight loss |
Real Success Stories
Numbers are great, but stories are what make the science feel reachable.
Case 1: Texas Patient, 45 y
In September 2020 a 45‑year‑old Texan showed up with a staggering HbA1c of 14.9 %. His doctor started him immediately on oral hypoglycemic agents while he began a rigorous lifestyle overhaul: low‑carb meals, daily walks, and nightly fasting after 8 p.m. Six months later his HbA1c was 7.2 % and he felt more energetic than he had in years.
Case 2: JB from Abuja
JB’s story is a textbook example of how diet can replace medication. Starting at 12.1 % HbA1c, he followed a 1500‑kcal, high‑fiber plan and trimmed his metformin dose from 60 mg to 30 mg within five weeks, eventually stopping it altogether. After three months his HbA1c was an astonishing 5.3 % — essentially normal.
Takeaway Checklist
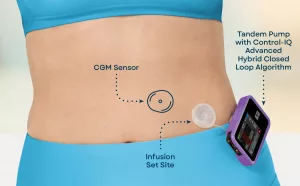
- Log blood glucose daily (or use a CGM for instant feedback).
- Weigh yourself weekly and note waist circumference.
- Schedule a medication review every 1–2 months until stable.
- Celebrate small wins – a lower fasting glucose, a new workout milestone, or a healthier food swap.
Monitoring Progress & Avoiding Pitfalls
How often should you test? If your HbA1c is above target, a test every three months keeps you on track. Once you’re stable for six months, move to a six‑month interval.
Many people wonder whether a lab HbA1c is the only way to gauge progress. Continuous glucose monitoring (CGM) can generate an estimated A1c (eA1c) after just 14 days, giving you an early signal if your plan is working. However, remember that eA1c can differ from the lab result if the sensor is miscalibrated.
Factors That Can Skew Results
- Hemoglobin variants (e.g., sickle‑cell disease).
- Severe anemia or recent blood transfusion.
- Kidney disease that alters red‑cell lifespan.
When any of these conditions exist, ask your clinician about alternative markers like fructosamine, which reflects glucose control over the past 2–3 weeks.
Lab HbA1c vs. eA1c vs. Fructosamine
| Metric | Timeframe | Pros | Cons |
|---|---|---|---|
| Lab HbA1c | 2–3 months | Gold standard | Delayed feedback |
| eA1c (CGM) | 2 weeks | Real‑time | Sensor accuracy needed |
| Fructosamine | 2–3 weeks | Fast | Affected by protein turnover |
Putting It All Together
Imagine your HbA1c as a garden. The soil (your genetics) may be set, but what you plant, how you water, and how often you weed determine the harvest. Low‑carb meals are the nutritious soil, exercise is the water, medication is the occasional fertilizer, and sleep/stress management are the weeds you pull out.
When each element works together, the garden flourishes – your numbers drop, your energy rises, and the risk of complications shrinks dramatically. The journey isn’t always linear; you might hit a plateau or a setback. That’s okay. Adjust, ask for help, and keep moving forward.
What’s your next small step? Maybe it’s swapping a sugary breakfast for a protein‑rich omelet, or scheduling a chat with your doctor about trying a weekly insulin like insulin efsitora. Whatever you choose, remember you’re not alone – millions have walked this path and come out healthier on the other side.
Conclusion
Lowering HbA1c isn’t a matter of magic pills alone; it’s a balanced blend of everyday choices, evidence‑based medication, and consistent monitoring. By understanding why HbA1c matters, adopting low‑carb, active, well‑rested habits, and selecting the right pharmacologic tools (whether it’s metformin, insulin glargine, or a weekly insulin option), you can achieve a safe, sustainable drop in your numbers. Real‑world stories prove that a 1–2 % reduction in as little as three months is possible – and every percentage point you shave off translates into a big win for your long‑term health.
If you’ve found a tip that resonates, try it today and watch the change unfold. And if you have questions, experiences to share, or just need a little encouragement, feel free to reach out. Your journey to a lower HbA1c—and a brighter, healthier future—starts now.






















Leave a Reply
You must be logged in to post a comment.