Did you know that up to 1 % of people worldwide develop painful nodules under their breast? If you’ve ever felt a burning, itchy lump that later turned into a painful abscess, you might be dealing with hidradenitis suppurativa breast. This guide cuts straight to the chase: what it looks like, why it happens, how to tell it apart from other breast problems, and the steps you can take to feel better fast. Grab a cup of tea, settle in, and let’s walk through it together.
Quick Facts
What is hidradenitis suppurativa (HS) and why does it show up on the breast?
What Is Hidradenitis Suppurativa?
HS is a chronic inflammatory skin disease that starts when hair follicles get blocked and inflamed, especially in areas rich in apocrine sweat glands. The breast, along with the armpits and groin, is a classic “friction zone” where skin rubs against skin, making it a prime spot for HS lesions.
How common is breast‑localized HS?
How Often Does It Occur?
Worldwide prevalence ranges from 0.00033 % to 4.1 % (JAAD study). In women aged 20‑30, especially those with larger breasts, obesity, or a smoking habit, the odds rise sharply. In fact, a recent Healthline overview notes that up to 1 % of HS patients develop lesions on the breast.
What are the hallmark symptoms?
Key Symptoms to Spot
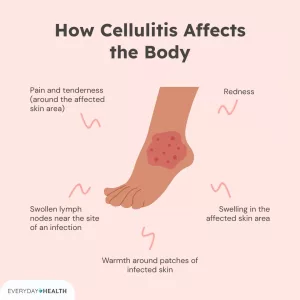
• Burning or itching that precedes a nodule
• Deep, painful nodules that may feel like a hard pea
• Rapid swelling, redness, or a warm feeling
• Progression to abscesses, sinus tracts (tiny tunnels), and scarring
• In some cases, lymphedema – a heavy, swollen feeling in the breast or chest wall
When should I see a doctor?
Red‑Flag Signs
If you notice fever, rapidly enlarging lesions, foul‑smelling drainage, or any suspicion of breast cancer (especially a new lump that doesn’t behave like typical HS), get medical help right away. Early diagnosis can prevent “tunnel” formation and long‑term scarring.
Diagnosis
How is HS on the breast distinguished from other breast conditions?
Differential Diagnosis
Below is a quick comparison to keep you from mistaking HS for something else:
| Condition | Typical Features | Key Differences |
|---|---|---|
| HS (breast) | Recurrent painful nodules, sinus tracts, often bilateral, lesions in other HS sites (axillae, groin) | Chronic, pattern of flare‑ups, tunnels under skin |
| Breast abscess (non‑HS) | Single, acute, often postpartum, localized swelling | No prior HS sites, usually resolves with antibiotics alone |
| Inflammatory breast cancer | Rapid skin thickening, peau d’orange, nipple retraction | Typically unilateral, no sinus tracts, systemic signs (weight loss) |
| Mastitis | Redness, warmth, often lactating women | Often resolves with simple antibiotics, no chronic tunnels |
What imaging and labs help confirm HS?
Useful Tests
• Ultrasound – Shows cystic‑like structures with low‑level echoes; a case report described a 17 mm × 11 mm fluid‑filled cavity under the nipple (PubMed case).
• MRI – Highlights skin thickening and tiny fluid collections in the periareolar zone.
• Blood work – CBC and CRP can gauge inflammation; cultures of drainage help rule out secondary infection.
Real‑world experience: a misdiagnosis story
Case Study Spotlight
In 2023, a 35‑year‑old woman presented with a painful periareolar nodule. Her surgeon first thought it was a simple breast cyst and planned drainage. After three unsuccessful procedures, a dermatologist recognized the pattern of HS (nodules in the axillae, groin, and now the breast) and started her on oral clindamycin + rifampin. Within weeks, the lesions softened, and the “tunnel” formation stopped. This story, published in J Surg Case Rep, highlights how easy it is to miss HS when it masquerades as a common breast issue.
When is a skin biopsy needed?
Biopsy Indications
If the presentation is atypical (e.g., a solitary breast lesion with no other HS sites) or cancer cannot be excluded, a punch biopsy shows follicular occlusion, neutrophilic infiltrate, and destroyed hair follicles – the classic HS fingerprint.
Treatment Options
What lifestyle tweaks can calm flare‑ups?
Everyday Adjustments
• Weight management – Reducing excess tissue lessens skin‑to‑skin friction.
• No smoking – Nicotine impairs wound healing and worsens inflammation.
• Clothing – Choose loose, breathable cotton bras; avoid underwire that rubs against lesions.
• Hygiene – Gentle antiseptic washes (chlorhexidine or benzoyl peroxide) keep the area dry and bacterial load low.
Which topical treatments work?
Topicals & Systemic Bridges
• Antiseptic washes (chlorhexidine) twice daily.
• Benzoyl peroxide 5 % gel to reduce follicular plugging.
• Topical clindamycin 1 % twice a day for mild inflammation.
When should oral antibiotics be introduced?
Oral Antibiotics
For moderate disease, a 2‑3 month course of doxycycline 100 mg twice daily works for many. For more stubborn lesions, clindamycin plus rifampin (300 mg/600 mg BID) has shown rapid improvement in clinical trials.
What about biologics for severe HS?
Biologic Therapy
Adalimumab (Humira) is the only FDA‑approved biologic for HS. The typical regimen starts with a loading dose (160 mg week 1, 80 mg week 2) followed by 40 mg weekly. Patients often notice a meaningful drop in pain after 12‑16 weeks. Discuss this option with a dermatologist experienced in HS, especially if you have recurrent abscesses or sinus tracts.
Are there procedural options?
Procedures & Surgery
• Intralesional steroids – Quick relief for a single painful nodule.
• Incision & drainage – Helpful for an acutely inflamed abscess but not a long‑term fix.
• CO₂ laser stripping – A less invasive alternative to wide excision (Lapins 1994).
• Wide surgical excision – The gold‑standard for severe, refractory disease. Healing may be by secondary intention or with skin grafts, but recurrence rates drop dramatically when the entire affected skin zone is removed.
How do I manage complications like scarring or lymphedema?
Complication Care
Scars can be softened with silicone gel sheets or scar massage. For lymphedema, a certified therapist can teach gentle compression and lymphatic drainage techniques. Rarely, chronic HS can turn into squamous‑cell carcinoma, so any new, non‑healing ulcer deserves a biopsy.
Can you see all of this in a single algorithm?
Treatment Flowchart
Below is a simple step‑by‑step roadmap you can keep on your phone:
| Step | What to Do | When to Move On |
|---|---|---|
| 1️⃣ Lifestyle | Weight loss, quit smoking, breathable bras, skin hygiene | If flare‑ups persist after 4 weeks |
| 2️⃣ Topicals | Clindamycin or benzoyl peroxide | After 6‑8 weeks without improvement |
| 3️⃣ Oral ABX | Doxycycline or clindamycin + rifampin | After 2‑3 months if lesions still active |
| 4️⃣ Biologics | Adalimumab (or other TNF‑α blocker) | If >3 months of systemic antibiotics fail |
| 5️⃣ Procedures | Steroid shots, I&D, laser, or surgery | For recurring abscesses, sinus tracts, or severe scarring |
Living with HS on the Breast
How do I keep everyday life comfortable?
Daily Comfort Tips
• Warm compresses (10‑15 min, 3×/day) soothe acute pain.
• Over‑the‑counter pain relievers (ibuprofen 400 mg) help inflammation.
• Use breathable bandages that keep the area dry after drainage.
• Swap underwire bras for soft, supportive sports bras during flare‑ups.
What about emotional well‑being?
Mental Health Matters
Living with visible nodules can shake confidence. Studies in the Journal of the American Academy of Dermatology link HS with higher rates of anxiety and depression. Reach out to a mental‑health professional, join online support groups (the HS Foundation has a lively forum), or simply share your story with a trusted friend. You’re not alone, and talking about it can lift a huge weight.
Is breastfeeding possible?
Breastfeeding Guidance
Most women with HS can safely breastfeed. Keep the affected area clean, wear a soft nursing bra, and discuss any systemic meds with your OB‑GYN. Biologics like adalimumab are considered compatible with breastfeeding by many experts, but always get individualized advice.
When might surgery be the right choice?
Surgical Decision‑Making
If lesions are extensive, cause constant drainage, or have led to significant scarring that interferes with daily life, a consultation with a breast‑plastic surgeon experienced in HS can map out a personalized excision plan. The goal is to remove diseased tissue while preserving as much breast contour as possible.
Bottom Line
Hidradenitis suppurativa on the breast is more than just an “annoying boil.” It’s a chronic condition that can disrupt comfort, self‑image, and even daily activities. The good news? With the right mix of lifestyle tweaks, topical and oral medicines, biologic therapy, and—when needed—surgical care, most people achieve lasting relief.
If you’re reading this and recognizing any of the signs, don’t wait. Talk to a dermatologist or a breast specialist today. And if you’ve already walked this path, share your experience in the comments—your story could be the beacon a fellow reader needs.
Would you like a printable version of the treatment flowchart? Click here to download. Feel free to reach out with questions; we’re all in this together.




















Leave a Reply
You must be logged in to post a comment.