Ever notice a cut that just won’t quit, no matter how many band‑aids you slap on it? That stubborn sore is what doctors call a chronic wound. In plain language, it’s a skin injury that hangs around longer than four weeks, refusing to follow the normal healing timetable.
Why does this happen, and more importantly, what can you do about it? Below we’ll walk through the science, the everyday impact, and the latest tools—including cutting‑edge gene‑therapy skin grafts—that can turn a never‑ending ulcer into a healed, healthy patch of skin.
What Makes Wounds Chronic
How Long Is Too Long?
Medical guidelines draw a pretty clear line: if a wound hasn’t shown signs of healing after 4–12 weeks, it’s considered chronic. This window isn’t arbitrary; it’s based on the normal phases of wound repair—hemostasis, inflammation, proliferation, and remodeling. When a wound stalls before it reaches the proliferative stage, the body essentially hits the pause button on healing.
Why Does Healing Stall?
Multiple factors can derail the healing orchestra. Below are the most common culprits:
- Impaired blood flow: Arterial blockages or venous reflux starve the wound of oxygen and nutrients.
- Metabolic hurdles: Diabetes, anemia, and malnutrition tug at the body’s repair machinery.
- Immune dysfunction: Persistent infection or bio‑film formation creates a hostile environment for new tissue.
- Mechanical stress: Re‑injury from pressure or shear keeps the wound in a perpetual state of inflammation.
According to a NIH overview, addressing these root causes is as vital as any dressing you might apply.
Types of Chronic Wounds
Chronic wounds aren’t a one‑size‑fits‑all condition. Their appearance, pain level, and underlying cause can differ dramatically. Below is a quick snapshot of the four major categories.
| Type | Typical Location | Key Cause | Characteristic Look |
|---|---|---|---|
| Pressure (Bed) Ulcers | Heels, sacrum, elbows | Prolonged pressure & shear | Red to purple skin, possible blister |
| Venous Leg Ulcers | Lower leg, ankle | Venous insufficiency | Irregular, shallow, with brownish skin |
| Diabetic Foot Ulcers | Ball of foot, toes | Neuropathy + poor circulation | Deep, often painless at first |
| Arterial Ulcers | Tips of toes, foot | Arterial blockage | Dry, painful, with well‑defined edges |
Pressure Ulcers
Imagine sitting on a rock for hours—your skin would start to turn pink, then sore. For people who spend most of their day in bed or a wheelchair, that “rock” is the constant pressure on a bony prominence. Risk factors include age, immobility, incontinence, and even obesity.
Venous Leg Ulcers
When veins can’t push blood back up the leg, fluid pools, skin swells, and eventually breaks down. You might notice a lingering ooze, a “stagnant” smell, or a darkened patch of skin. These ulcers love the lower leg because gravity does the heavy lifting.
Diabetic Foot Ulcers
Diabetes messes with two things you need for healing: sensation and circulation. A tiny pebble can become a deep wound, and because nerves are dulled, you might not even feel it until infection sets in. This is why regular foot checks are a lifeline for anyone living with diabetes.
Arterial Ulcers
These are the “dry‑fire” cousins of chronic wounds—painful, often sharp, and located on the tips of toes where blood flow is poorest. If you notice a wound that hurts even when you barely touch it, ask your doctor to check arterial supply.
Impact on Daily Life
Physical & Emotional Toll
A chronic wound isn’t just a skin problem; it’s a daily reminder that something is wrong. Pain can range from a dull ache to a burning sting, limiting walking, climbing stairs, or even tying shoes. The constant worry about infection can breed anxiety, and isolation creeps in when you avoid social outings for fear of “showing” the wound.
Economic Burden
Every dressing change, clinic visit, and specialist appointment adds up. In Australia, the NSW Chronic Wound Management Initiative reported that chronic wounds account for a significant portion of healthcare spending, not to mention lost work days and caregiver hours.
Standard Care Pathway
Assessment & Debridement
The first step is a thorough assessment—size, depth, tissue type, and signs of infection. Debridement (removing dead tissue) can be done with a scalpel, enzymatic agents, or even specialized dressings that “eat” away necrotic material. Clean the wound with sterile saline; studies still debate the superiority of saline versus other solutions, but saline remains the most widely accepted choice (NIH).
Dressings & Moist‑Healing
Remember the “Goldilocks” principle? Too dry slows cell migration; too wet dissolves new tissue. Modern dressings—hydrocolloids, foams, alginates—maintain that sweet spot. They also act as a barrier against bacteria while allowing oxygen to pass.
Adjunct Therapies
When standard dressings aren’t enough, clinicians turn to advanced options:
- Negative‑Pressure Wound Therapy (NPWT): A vacuum pump draws out excess fluid, promoting granulation.
- Topical Oxygen Therapy: Delivers high‑concentration oxygen directly to the wound bed, boosting cellular activity.
- Gene‑Therapy Skin Grafts: By inserting corrected genes into skin cells, these grafts can jump‑start healing in resistant wounds. Learn more about gene therapy skin grafts.
- Dystrophic Epidermolysis Bullosa (DEB): A rare genetic skin condition that creates chronic blisters. Advanced grafts and cellular therapies are changing outcomes for DEB patients. See the discussion on genetic skin condition.
Lifestyle & Self‑Management Tips
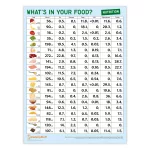
Nutrition for Repair
Think of your body as a construction site—without the right materials, the scaffolding collapses. Aim for 1.2–1.5 g of protein per kilogram of body weight daily, and don’t forget vitamin C, zinc, and omega‑3 fatty acids. A simple “healing plate” might include grilled salmon, quinoa, leafy greens, and a handful of berries.
Foot & Skin Care Routine
Check your feet every morning—look for redness, calluses, or broken skin. Keep nails trimmed, wear well‑fitted, breathable shoes, and moisturize the surrounding skin (avoid the wound itself to prevent maceration). For those with DEB or other blistering disorders, gentle handling is essential; read about managing blistering skin disease for detailed tips.
When to Call a Professional
Set up a red‑flag checklist:
- Increasing pain or spreading redness
- Foul odor or pus
- Rapid size change or deepening
- Fever, chills, or unexplained fatigue
If any of these appear, schedule a visit promptly—early intervention dramatically improves outcomes.
Supporting Your Mental Health
Chronic pain can feel like a “painful dermatologic disease” that eats away at confidence. Talking to a therapist, joining a support group, or simply sharing your story with a trusted friend can lighten the emotional load.
Future Directions – Emerging Therapies
Science never sleeps, and the horizon for chronic wound care is bright. Here are a few developments that might become mainstream in the next few years:
- CRISPR‑based skin regeneration: Gene editing directly in the wound bed aims to correct underlying genetic defects and stimulate rapid tissue growth.
- Smart dressings with sensors: Tiny electronics monitor pH, oxygen, and bacterial load, sending real‑time data to your phone or clinician.
- Tele‑wound‑care platforms: High‑resolution photos and AI analysis help clinicians adjust treatment without a physical visit—particularly helpful for rural patients.
According to recent NIH‑funded trials (2023‑2025), combining these technologies with traditional care could cut healing times by up to 40 %.
Conclusion
Chronic wounds are more than just stubborn cuts; they are signals that something in the body’s healing orchestra is out of tune. By recognizing the warning signs early, addressing underlying health issues, and using the right dressings—plus, when needed, advanced tools like painful dermatologic disease therapies—you can guide that discord back into harmony.
Remember, you’re not alone in this journey. Whether you’re checking your feet, tweaking your diet, or exploring new treatments, each small step brings you closer to a healed, healthier skin. If you have questions or want to share what’s worked for you, feel free to reach out. Together, we can turn chronic wounds from a daily burden into a story of recovery.






















Leave a Reply
You must be logged in to post a comment.