Let’s cut to the chase: IVF itself does not push your body into early menopause. What can happen, though, is that the hormonal fireworks of an IVF cycle sometimes feel a lot like the early stages of menopause, leaving you wondering if the treatment you hoped would bring a baby is actually stealing your future fertility.
Understanding the real risks and the genuine causes of early menopause lets you make smarter choices, keep your peace of mind, and stay in control of your family‑building journey. So grab a cuppa, settle in, and let’s untangle the facts together.
How IVF Works
What IVF Actually Is
In‑vitro fertilisation (IVF) is a series of steps that lets doctors create embryos outside the body and then place them back into the uterus. The basic roadmap looks like this:
- Ovarian stimulation – you take fertility drugs to coax your ovaries into producing multiple eggs.
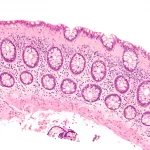
- Egg retrieval – a minor surgical procedure pulls the mature eggs from your ovaries.
- Fertilisation – sperm meets the eggs in a lab dish; the resulting embryos grow for a few days.
- Embryo transfer – one or more embryos are gently placed into your womb.
Which Hormones Are Used and Why
During stimulation you’ll likely be prescribed a cocktail of follicle‑stimulating hormone (FSH), sometimes combined with luteinising hormone (LH), and later a “trigger” shot of human chorionic gonadotropin (hCG) to finish egg maturation. Some clinics add GnRH‑antagonists or agonists to keep your body from going into a natural ovulation cycle too early.
Typical Dosage & Duration
Most protocols last 10‑12 days, with daily injections ranging from 150‑450 IU of FSH. The exact amount depends on age, ovarian reserve, and previous response to medication.
IVF Success Rates by Age
| Age | Live Birth Rate per Cycle |
|---|---|
| Under 35 | ≈ 40‑45 % |
| 35‑37 | ≈ 30‑35 % |
| 38‑40 | ≈ 20‑25 % |
| 41‑42 | ≈ 12‑15 % |
| Over 42 | ≈ 5‑10 % |
These numbers come from the UK’s Human Fertilisation & Embryology Authority (HFEA) 2023 report, which noted 69,000 IVF cycles for 53,000 patients that year.
IVF & Menopause?
What the Research Says
A 2021 peer‑reviewed article in International Journal of Women’s Health examined whether IVF shifts the timing of natural menopause. The researchers found no statistically significant difference between women who underwent IVF and matched controls – the “menopause clock” kept ticking at its usual speed.
Why IVF Hormones Can Feel Like Menopause
The same high doses of estrogen‑modulating drugs that push your ovaries to make extra eggs also create a temporary hormonal roller‑coaster. You might notice:
- Hot flashes or night sweats
- Mood swings or brain fog
- Weight fluctuations
- Bloating and mild headaches
- Irregular periods or spotting after the cycle
These symptoms overlap with perimenopause, which is why many women mistakenly think IVF has “jump‑started” early menopause.
Real‑World Numbers
Survey data from several UK clinics suggest roughly 5 % of IVF patients report menopause‑like symptoms during or shortly after treatment. Importantly, most see these symptoms resolve within a few months once the hormone regimen stops.
The Bottom Line for You
IVF does not strip your ovaries of a whole year’s worth of eggs, and it does not accelerate the natural decline of ovarian reserve. What it can do is temporarily mimic menopause, which can be unsettling but is usually short‑lived.
Early Menopause Causes
Medical Triggers
True early menopause (before age 45) often stems from:
- Genetic predisposition – a family history of early menopause.
- Autoimmune disorders – the body attacks its own ovarian tissue.
- Chemotherapy or radiotherapy – especially for cancers affecting the pelvic area.
- Surgical removal of both ovaries (oophorectomy).
These factors are outlined by the NHS early menopause page, which also emphasizes that the condition affects roughly 1 in 8 women.
Lifestyle Influences
While you can’t change your genetics, you can tweak some habits:
- Smoking – nicotine speeds up ovarian ageing.
- Low body weight or extreme dieting – reduces estrogen production.
- Very early menarche (first period before age 8) – associated with earlier ovarian exhaustion.
Spotting the Difference
How do you know whether you’re dealing with hormone‑related side‑effects from IVF or true early menopause? Consider timing and testing:
- Timeline – IVF‑related symptoms usually appear during or within three months of a cycle and fade thereafter.
- Blood work – Elevated follicle‑stimulating hormone (FSH) and low anti‑Müllerian hormone (AMH) persisting for six months or more point toward genuine early menopause.
IVF Risks & Side‑Effects
Common Short‑Term Effects
Most women experience mild discomfort:
- Bloating and pelvic pressure from the ovaries swelling.
- Minor cramping after egg retrieval.
- Emotional ups and downs as hormone levels swing.
Serious (but Rare) Risks
| Risk | What It Looks Like | Incidence |
|---|---|---|
| Ovarian Hyperstimulation Syndrome (OHSS) | Severe abdominal pain, rapid weight gain, shortness of breath | ≈ 1‑2 % of cycles (moderate‑severe) |
| Multiple pregnancy | Twins or more; higher chance of preterm birth | ≈ 15‑25 % when >1 embryo transferred |
| Ectopic pregnancy | Implantation outside the uterus | ≈ 2 % of IVF pregnancies |
| Egg‑retrieval injury | Bleeding or infection from the needle | Very rare (< 0.5 %) |
How These Risks Touch Menopause Health
If estrogen stays low for a prolonged period after a cycle (for instance, if you’re unable to conceive and stop hormone support), you could see bone‑density loss or a slight increase in cardiovascular risk – the same concerns that affect any woman in early menopause. Hormone replacement therapy (HRT) can safely bridge that gap under a doctor’s guidance.
Fertility Options After Early Menopause
Frozen Eggs or Embryos
If you happened to bank eggs or embryos before the menopause‑like transition, you can still use them. Success rates hover around 30‑40 % per transfer for women under 40 at the time of freezing.
Donor‑Egg IVF
When your own eggs are no longer viable, donor eggs become the gold standard. The HFEA reports a live‑birth rate of about 45‑55 % per cycle when using fresh donor eggs, making it a reliable path to parenthood.
Surrogacy
If your uterus can’t carry a pregnancy (for instance, after a hysterectomy), a surrogate can gestate the embryo created from donor eggs and your partner’s sperm (or donor sperm). This route is legally regulated in the UK and offers a hopeful option for many.
Decision‑Making Checklist
- Medical suitability – hormone levels, uterine health.
- Emotional readiness – counseling can help process grief and excitement.
- Financial planning – IVF, donor cycles, and surrogacy each carry distinct costs.
- Legal considerations – especially for surrogacy, ensure contracts are in place.
Expert Insights & Authoritative Sources
Quotes from Specialists
Dr. Erika Schwartz, a reproductive endocrinologist quoted in several media pieces, notes: “The hormonal milieu of IVF can mimic perimenopausal symptoms, but it doesn’t deplete the ovarian reserve beyond the cohort of eggs that would have been ovulated naturally in a year.”
Psychiatrist Dr. Maya Patel adds, “Women who think IVF has forced them into early menopause often experience anxiety. A clear medical explanation and a supportive counsellor can dramatically reduce that stress.”
Key Data Sources to Trust
When you need hard numbers, turn to:
- The 2021 study in International Journal of Women’s Health on IVF and menopause timing.
- NHS guidance on early menopause and its treatment options.
- HFEA annual reports for up‑to‑date IVF success statistics.
- Professional societies such as the British Menopause Society for lifestyle and hormone‑therapy recommendations.
Real‑World Stories (Experience)
Case Study 1 – “Three Cycles, No Early Menopause”
Sarah, 38, completed three IVF attempts using her own eggs. She reported hot flashes and mood swings during the first stimulation, but blood tests three months later showed normal FSH and a healthy AMH level (2.3 ng/mL). Her doctor reassured her that the symptoms were medication‑related and not an indication of early menopause.
Case Study 2 – “Celebrity Headline vs. Science”
In 2023, Trinny Woodall’s story made headlines suggesting 16 IVF rounds “triggered” her early menopause. However, the same year a review of large‑scale IVF data found no causal link. The discrepancy highlights how personal anecdotes can sometimes outshine evidence – a reminder to always check the science.
What I Wish I’d Known
- Hormone side‑effects are temporary; they don’t mean permanent loss.
- Regular blood work after IVF can put any lingering doubts to rest.
- Being proactive about lifestyle (quit smoking, maintain a healthy weight) can delay true early menopause.
Practical Tips & Monitoring
Track Your Ovarian Reserve
Before starting IVF, ask for an AMH test and an antral follicle count (AFC). Repeat these tests six months after your cycle to see if anything has truly shifted.
Healthy Habits That Protect Ovaries
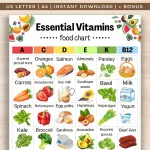
- Eat a balanced diet rich in calcium, vitamin D, and omega‑3 fatty acids.
- Engage in regular weight‑bearing exercise – it supports bone health.
- Avoid smoking and limit alcohol, both of which can accelerate ovarian ageing.
- Manage stress through mindfulness, yoga, or therapy; chronic stress can disturb hormone balance.
When to Call a Specialist
If you notice any of the following, schedule a visit:
- Irregular periods persisting beyond three months after an IVF cycle.
- Persistent hot flashes, night sweats, or mood changes.
- Blood test results showing FSH > 30 IU/L or AMH < 0.5 ng/mL.
Conclusion
Here’s the short version: IVF does not cause early menopause, but the hormonal surge that fuels egg production can temporarily make you feel like you’re entering the menopausal transition. True early menopause has its own set of medical, genetic, and lifestyle causes, and it can be managed with the right blend of medical care and healthy living.
If you’re eyeing IVF, talk openly with your fertility specialist about your hormone levels and any menopause‑like symptoms you experience. Keep an eye on your ovarian reserve, and don’t hesitate to ask for blood tests if something feels off. Remember, you’re not alone – many women have walked this path, and a supportive medical team can help you navigate both the joys and the anxieties.
Got questions or personal stories about IVF and early menopause? Share them in the comments or reach out to a trusted fertility counsellor. Knowledge, empathy, and a little bit of optimism go a long way on the road to parenthood.























Leave a Reply
You must be logged in to post a comment.