
Wait, Why Are We Even Talking About This?
Okay, so you head to the doctor for a nagging sinus infection or maybe something “down there” is just feeling off after a few tough workouts (raise your hand if you live in yoga pants—I see you!). The doc scribbles out a prescription, you grab your antibiotics… and a few days later, boom. Unwelcome visitor. Not the fun kind. Yeast infection.
It’s honestly amazing how nobody warns you about this in health class, right? One day you’re trying to kill bad bacteria with antibiotics, and the next you’re Googling “why am I SO itchy?” or “is this cottage cheese discharge normal?” (Seriously, whoever came up with that analogy? Oof.)
This topic comes up so much in wellness circles—and at every brunch with close friends—that I figured it was time we had a real talk about the list of antibiotics that cause yeast infections and what in the world you can do about it. If you ever wondered why some meds seem to swap one problem for another… trust me, you are SO not alone.
Inside Story: Why Antibiotics Mess with Your Vibe
Let’s break it down like this: your vaginal area (and honestly, most of your body) is kind of like a little ecosystem. You’ve got tons of good bacteria—especially these superstar guys called Lactobacillus—who work hard to keep yeast like Candida in check. If everything’s balanced, you’re golden. But antibiotics? They’re like dropping a bomb on the whole community, blasting away ALL bacteria—good and bad—sometimes leaving the yeast to party unchecked.
So, cue the classic signs: relentless itching, burning (especially during a workout or after, ouch!), thick white discharge that can legit look like ricotta cheese, and just general “I am not okay” vibes. According to research on why antibiotics sometimes lead to yeast infections, this is sadly very normal, especially for women aged 15-44, but honestly, it can happen at any age or gender. Love that equality, right?
Quick Check: Ever Noticed This?
Have you ever wrapped up a round of antibiotics—maybe after strep throat, UTI, or that pesky post-travel infection—only to be ambushed by a weird, persistent itch or some next-level discomfort? Yup. Up to 30% of women report yeast infections during or after antibiotics (findings on yeast infections from GoodRx). You might be glad you kicked the original infection, but suddenly you’re camping out in the pharmacy aisle scanning antifungal creams.
One friend of mine, Ali, swears she can set her calendar by it: sinus infection in January, yeast infection in February. It’s basically a tradition at this point. So if you’re silently nodding—yeah, totally normal.
Who’s Most At Risk?
Honestly… anyone with a vagina. (Sorry, ladies.) But the risk goes up if:
- You’re pregnant or taking hormonal birth control (hormones can do wild things, not always fun).
- You have diabetes, especially if it’s not perfectly managed.
- Your immune system’s been knocked down (think: chemo, HIV, chronic illness).
- You’re on super strong or long courses of antibiotics. Broad-spectrum meds can do the most damage here. More on that in a sec.
Let’s not forget: men can get yeast infections, too—especially in the groin. But for the rest of this article, I’ll mostly talk vagina, since that’s where the majority of drama happens.
The Usual Suspects: Which Antibiotics Cause Yeast Infections?
Ready for the inside scoop? Here’s the list of antibiotics that cause yeast infections most often—and believe me, they’re pretty common.
| Antibiotic Group | Common Examples | Usual Uses | Risk of Yeast Infection |
|---|---|---|---|
| Penicillins | Amoxicillin, Ampicillin | Ear infections, dental work, UTIs, strep throat | High |
| Cephalosporins | Cephalexin, Cefuroxime | Respiratory infections, skin/bone infections | High |
| Tetracyclines | Doxycycline, Minocycline | Acne, UTIs, respiratory, Lyme disease | High |
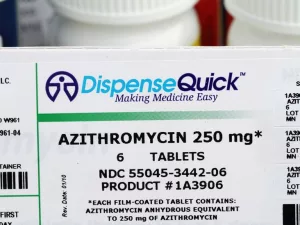
| Macrolides | Azithromycin (“Z-Pak”), Clarithromycin | Bronchitis, pneumonia, sinus infections | Moderate |
| Fluoroquinolones | Ciprofloxacin, Levofloxacin | UTIs, respiratory infections | High |
Notice amoxicillin’s right up top? Not just “Can amoxicillin cause yeast infection.” It straight up does for a lot of folks. If you’re curious about how this happens or want real stories, you’ll love reading about Can amoxicillin cause yeast infection—it feels oddly comforting to know exactly what to expect before opening that pharmacy bottle.
But… Why Are These Ones So Bad?
It all comes down to “broad spectrum.” That means these antibiotics don’t just target the bad apple bacteria; they take out a bunch of innocent bystanders, too. Once your good Lactobacillus is gone, yeast like Candida can take over in days (see what Healthline says on losing healthy bacteria).
Tetracyclines (like doxycycline) and fluoroquinolones (cipro, levofloxacin) are especially notorious, whether you’re taking them for acne, travel bugs, UTIs, or respiratory junk. Also? Macrolides such as azithromycin fly a little under the radar, but more and more people report trouble with them.
I had a blast (read: not) with doxycycline years ago—the acne cleared, but the aftermath in my yoga practice was… not cute.
How Yeast Takes the Lead: A Mini Microbiome Story
Imagine your vagina’s healthy mix of bacteria and yeast is like a gardener tending her plot. Antibiotics? They’re a freak hailstorm. Left in the aftermath, those super-resilient yeast plants (Candida!) grow wild while your helpful bacteria are recovering. (I swear my biology teacher should’ve taught this instead of frog dissections… would’ve made more sense for real life.)
Symptoms You Can’t Ignore
Here’s what might tip you off that antibiotics kicked off a yeast infection:
- Itching and burning—not just a “maybe I need different underwear” itch, either.
- Thick, white discharge (cottage cheese, but not the good-for-you kind).
- Pain or burning with sex or peeing.
- Redness and swelling—sometimes just walking feels “off.”
A lot of folks (myself included) will try to tough it out. But listen: there’s no reason to just accept discomfort. Especially because the solutions are pretty reasonable.
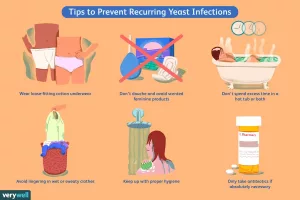
Can You Do Anything To Prevent This? (Spoiler: Yes!)
This isn’t all doom and gloom! If you know you’re stuck taking one of the list of antibiotics that cause yeast infections (and sometimes you just have to), there are a few tricks that can seriously help.
Don’t Skip Probiotics—Your Future Self Will Thank You
If you take only one thing from this article, let it be this: start a daily probiotic as soon as you grab your prescription. Yogurt with live cultures, kefir, or probiotic supplements can help restore those good Lactobacillus bacteria (find tips on restoring balance at Medical News Today). Some women swear by this hack. I’ve tried it myself and—honestly—no yeast infection after a two-week course of cephalexin? Magic.
(Of course, ask your doctor or pharmacist about timing, especially if you’re taking specific antibiotics. You don’t want the probiotic to just get nuked too soon!)
Diet, Hygiene, All The Little Things
- Swap tight synthetic workout clothes for loose, breathable cotton (rewash after sweaty gym sessions—trust me).
- Change out of wet swimsuits asap (perfect storm for yeast overgrow).
- Skip douches, scented soaps, or wipes.
- Cut back on sugar if you’re really prone—yeast loves a sugar party.
There’s a great in-depth look at this over on Can you treat a yeast infection while on antibiotics—worth the bookmark if you’re in the thick of it.
But What If You Still Get a Yeast Infection?
No shame, no drama—it happens, even with the best prevention! If you feel symptoms coming on, it’s okay to finish your antibiotic (unless your doctor says otherwise—safety first). The next step? Head to the pharmacy for an over-the-counter antifungal cream (like miconazole or clotrimazole). For more stubborn or recurring cases, you may need a prescription pill—typically fluconazole (GoodRx on treatment options).
Also useful: see your doctor if this is your first yeast infection, things don’t clear up quickly, or symptoms are severe. Sometimes it’s actually another vaginal infection masquerading as a yeast problem—and treatments are totally different.
If you’re pregnant, diabetic, get more than four yeast infections a year, or have a weakened immune system: definitely loop in your provider early. The risk of complications is higher and you might need a different game plan.
Side Note: Can You Take Both Meds?
Short answer—yep! You can absolutely treat a yeast infection while you’re still on antibiotics (sometimes you have to). Curious about timing, safety, or juggling both? Definitely check out can you treat a yeast infection while on antibiotics. It covers everything from pharmacist advice to pro tips for managing your meds like a boss.
Does This Happen to Everyone?
Not everyone will get a yeast infection from antibiotics, and you never know exactly how your body will react to a certain drug until you try it. But if you have a history of yeast infections, your chance definitely goes up. The good news? Now you know what to watch for and how to dodge it!
Final Thoughts: Take Control—No Shame, No Judgment
Here’s what I hope you remember: antibiotics are awesome for kicking infection… but they can absolutely shake up your body’s balance. The list of antibiotics that cause yeast infections isn’t a reason to panic—just a heads-up to be proactive.
Start those probiotics, eat some yogurt, wear comfy clothes, and don’t feel awkward bringing up concerns with your doctor. If you do get a yeast infection (even if it’s, like, immediately after amoxicillin), there’s help—real fast. If you want to get into the nitty-gritty, or you’re already dealing with one, swing by Can amoxicillin cause yeast infection and Can you treat a yeast infection while on antibiotics—it’ll save you from some messy, late-night Google spirals.
Stay curious, listen to your body, and never be embarrassed to talk about this stuff. We’re all out here just trying to stay sane, strong, and yeast-free. Now—go live your best life (and here’s hoping your antibiotics work fast and your probiotics work even faster!).





















Leave a Reply
You must be logged in to post a comment.