First thing’s first – you’ve probably heard a lot of medical‑sounding terms and wonder, “Will I feel terrible on Pluvicto?” The short answer is: many patients experience side effects, but most of them are predictable, manageable, and often short‑lived. Knowing what to expect lets you stay in control, keep the treatment working, and focus on the big picture – beating prostate cancer.
In this guide I’m walking you through the side‑effect landscape, how the dosage plan fits in, ways to keep uncomfortable symptoms at bay, and even the cost side of things. Think of it as a friendly coffee chat with a well‑informed companion who’s been through the paperwork, the labs, and the “what‑now?” moments.
Why It Matters
Pluvicto (lutetium‑177 vipivotide tetraxetan) is a radioligand therapy for metastatic castration‑resistant prostate cancer (mCRPC). It delivers targeted radiation straight to cancer cells that express the PSMA protein. That precision is a huge win, but the radiation can also affect healthy tissue – especially bone marrow and kidneys. Understanding the side‑effect profile helps you and your care team decide when to pause, lower, or continue the dose, and it reduces the chance of an unexpected emergency.
According to a recent FDA safety briefing, about 71 % of patients report at least one grade ≥ 2 adverse event, yet with proactive monitoring, most stay on schedule FDA safety update. The goal isn’t to scare you; it’s to empower you with the knowledge that makes you an active participant in your treatment.
Common Side Effects
These are the “every‑day” aches, pains, and quirks most folks notice in the first few weeks. They’re usually mild to moderate, and they often improve with simple home measures.
| Side Effect | How Common | Typical Onset | Quick Relief Tips |
|---|---|---|---|
| Fatigue / Tiredness | ≈ 70 % | Within 1‑2 weeks | Gentle walks, short naps, stay hydrated |
| Dry Mouth | ≈ 55 % | Day 1‑3 post‑infusion | Sugar‑free gum, sip water every 15 min |
| Nausea & Vomiting | ≈ 45 % | First infusion | Prescribed anti‑emetic (ondansetron), small bland meals |
| Loss of Appetite | ≈ 40 % | 1‑2 weeks | High‑calorie shakes, eat 5‑6 small meals |
| Diarrhea / Constipation | ≈ 30‑40 % | Ongoing | Fiber supplement, plenty of fluids, stool softener if needed |
| Low Red Blood Cell Count (Anemia) | ≈ 25 % | 3‑6 weeks | Iron‑rich foods, possible ESA therapy (talk to oncologist) |
| Low Platelet Count (Thrombocytopenia) | ≈ 20 % | 4‑8 weeks | Avoid NSAIDs, monitor CBC before each cycle |
| Urinary‑Tract Infection | ≈ 15 % | Variable | Hydration, prompt antibiotics if fever or burning |
How to Self‑Manage Mild Symptoms
Think of your body like a garden. When a new plant (Pluvicto) is introduced, you’ll notice a few weeds sprouting. Pull them out early, and the garden thrives.
- Hydration is king. Aim for at least 2 liters of water a day, and keep a water bottle on your bedside table.
- Track everything. Use a simple notebook or a phone app to log fatigue levels, mouth dryness, and any new bruises. Share the log with your nurse before each appointment.
- Don’t self‑medicate blindly. Over‑the‑counter pain relievers can hide fevers, which are red flags for infection. Always ask your doctor before taking ibuprofen or aspirin.
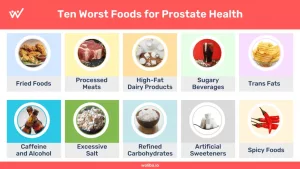
- Eat smart. Soft, nutrient‑dense foods (yogurt, oatmeal, avocado) are easier on a dry mouth and can keep calories up despite a reduced appetite.
Serious Side Effects
These are the ones that merit an immediate call to your care team or a trip to the emergency department. They’re rarer, but being able to spot them early can be lifesaving.
| Red‑Flag Symptom | Why It Happens | When to Seek Help |
|---|---|---|
| Black, tarry stools (melena) | Gastrointestinal bleeding | Any occurrence – call oncologist ASAP |
| Blood in urine or cloudy/red urine | Bladder irritation or bleeding | Immediately |
| Severe fatigue with easy bruising | Myelosuppression (grade ≥ 3) | When you notice new bruises or feel unusually weak |
| Sudden drop in urine output or flank pain | Kidney injury | Within 48 hours of symptom onset |
| Hives, swelling of face/lips, trouble breathing | Allergic reaction | Call 911 right away |
| Tingling, peripheral edema, blurred vision | Rare neurological or vascular effects | Prompt evaluation |
When to Call 911
If you experience any of the following, treat it like a fire alarm – act fast:
- Difficulty breathing or throat swelling
- Chest pain that doesn’t go away
- Severe vomiting with coffee‑ground appearance
- Uncontrolled bleeding (gums, rectum, or any puncture)
Dose‑Modification Guidelines (Expert Insight)
The official prescribing information recommends:
- Grade 2 myelosuppression: Hold the next dose until labs improve to Grade 1 or baseline.
- Grade ≥ 3: Hold the dose, then reduce the planned dose by 20 % (from 7.4 GBq to 5.9 GBq). If severe toxicity recurs, discontinue treatment.
- Renal toxicity: Withhold and reassess kidney function; dose may be reduced or stopped based on severity.
These rules keep the therapy effective while protecting your blood line and kidneys. Discuss any lab changes with your oncologist – they’ll know whether a brief pause or a dose tweak is right for you.
Dosage & Schedule
Pluvicto is given as an intravenous infusion of 7.4 GBq (200 mCi) every six weeks, up to six cycles, unless disease progression or intolerable toxicity occurs. The six‑week interval isn’t arbitrary; it gives bone marrow time to rebound after radiation exposure.
Special populations (mild‑to‑moderate renal or hepatic impairment, patients 65 years and older) generally do not require dose adjustments, but the treating center will still run daily kidney and liver function tests American Cancer Society guidelines. If you have a history of kidney disease, your doctor may add extra hydration instructions before and after infusion.
Impact of Timing on Toxicity
Data from the pivotal VISION trial showed a modest rise in Grade ≥ 3 myelosuppression after the third and fourth cycles, then a plateau. That means the first two infusions are often the “learning curve,” and close monitoring during cycles three‑four is key.
Questions to Ask Your Doctor About Dose
- “If my blood counts drop, can we safely reduce the next dose?”
- “How often will you repeat CBC, kidney, and liver tests?”
- “What’s the plan if I develop a serious side effect after cycle 2?”
Managing Side Effects
Now that you know what might show up, let’s talk about the toolbox you can use every day.
Hydration & Renal Safety
Drink at least 2 L of clear fluids daily, and empty your bladder often. Some centers give you a hydration protocol the day of infusion (e.g., 500 ml of saline before the dose and 1 L of oral fluids afterward). This flushes out residual radioactivity and eases kidney load.
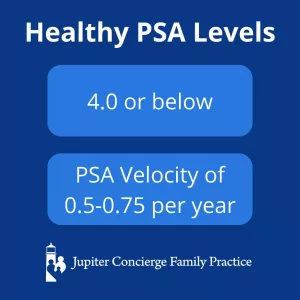
Blood‑Count Monitoring
Before each infusion you’ll get a complete blood count (CBC). If your neutrophils or platelets dip below the protocol‑defined thresholds, the team may hold the dose or give growth‑factor support (filgrastim). Keep a copy of each lab report; it’s your passport for the next cycle.
Gastro‑Intestinal Comfort
Anti‑emetics are standard – ask if you can take them the night before. For constipation, a gentle fiber supplement (psyllium) plus a stool softener works well. Diarrhea? Oral rehydration solutions and a bland BRAT diet (bananas, rice, applesauce, toast) often tame it.
Oral Health & Dry Mouth
A dry mouth can feel like a desert. Chewing sugar‑free gum, sucking on ice chips, and using a saliva substitute spray keep the moisture level up. Visit your dentist before starting Pluvicto and let them know you’re on a radiopharmaceutical – they may schedule extra cleanings.
Psychological Support
The emotional roller coaster is real. Many patients benefit from counseling, support groups, or even brief mindfulness apps. A study in PubMed found that participants who joined a peer‑support network reported lower anxiety scores during treatment.
Downloadable Checklist
Below is a quick “Before Your Next Appointment” checklist you can print out or keep on your phone:
- Bring latest CBC, kidney, and liver labs
- Note any new symptoms (fatigue level, mouth dryness, fever)
- Have a list of current meds, including vitamins
- Prepare questions about dose adjustments or side‑effect meds
- Check insurance pre‑authorization status
Cost & Insurance
Pluvicto isn’t cheap – the average wholesale acquisition cost hovers around $30,000 – $35,000 per dose in the United States. That can add up quickly with six cycles. However, most patients access the drug through Medicare Part B, and many pharma companies offer patient‑assistance programs.
Here are a few practical steps to lessen the financial strain:
- Pre‑authorization. Your oncology office usually handles this, but double‑check the paperwork before each cycle.
- Check for co‑pay assistance. Novartis runs a “Patient Support Program” that can cover a portion of the cost for eligible individuals.
- Ask about “bundled” pricing. Some hospitals negotiate a flat rate for the entire 6‑cycle course.
- Use a cost‑estimator tool. Websites like GoodRx provide up‑to‑date pricing across pharmacies – just search “Pluvicto” and compare.
Financial Toxicity & Side‑Effect Care
When out‑of‑pocket costs rise, patients sometimes skip supportive meds (like anti‑emetics) or delay lab work, which can worsen side effects. Discuss any financial worries early with your social worker; they can connect you to grants, charity funds, or state assistance programs.
Real Patient Stories
Stories are the glue that turns data into something we can feel. Below are two quick snapshots (names changed for privacy) that illustrate how people have navigated the side‑effect journey.
John, 68 – “Hydration Saved My Kidneys”
John was diagnosed with mCRPC two years ago. After his third Pluvicto infusion, his blood work showed a rising creatinine level. His nurse reminded him to drink an extra 1 L of water each day and to use a bedside urination reminder. Within a week his kidney markers normalized, and his next dose proceeded without a hitch.
Maria, 71 – “The Dry‑Mouth Hack”
Maria struggled with a persistently dry mouth that made eating painful. She tried sugar‑free gum but found it insufficient. After a dietitian visit, she started sipping warm herbal teas and using a saliva‑stimulating lozenge (xylitol‑based). The simple habit reduced her dryness by about 60 % and let her regain weight lost during treatment.
What about you? Have you found a particular tip that made a difference? Drop a comment – your experience could help the next person reading this page.
Bottom Line & Next Steps
Pluvicto side effects are a mixed bag: the common, manageable ones keep you on track, while the serious, rarer ones need swift action. By staying hydrated, tracking labs, communicating openly with your oncology team, and leaning on financial‑aid resources, you can maximize the benefit of this powerful therapy without letting side effects steal the spotlight.
Take a moment now: print the symptom‑tracker table, add your questions to the checklist, and set a reminder to call your nurse if anything feels “off.” You’ve got the knowledge; now you have the plan.
Remember, you’re not alone in this journey. Your medical team, support groups, and even strangers on forums are all part of the same crew, cheering you on toward a future where prostate cancer is just a chapter, not the whole story.



















Leave a Reply
You must be logged in to post a comment.