Imagine you hear the word “rubella” and think, “Just another mild childhood rash, right?” Most of us do. The truth is a bit more nuanced. Rubella itself often feels like a brief, itchy blush that fades in a few days, but the danger lies in who catches it and when. For pregnant people, especially in the first trimester, the virus can turn a routine infection into a life‑changing event for both mother and baby.
In this article I’ll walk you through how rubella spreads, why the stakes are highest during pregnancy, what other complications can pop up, and—most importantly—how you can protect yourself and your loved ones. Think of it as a friendly coffee‑chat where I share the facts I’ve gathered from CDC guidelines, real‑world stories, and a dash of personal experience.
How It Spreads
Rubella is a virus that loves to hitch a ride on tiny droplets expelled when someone coughs, sneezes, or even talks loudly. You can also pick it up by touching a contaminated surface and then your eyes, nose, or mouth. The tricky part? A person can be contagious seven days before a rash appears and remains so for about a week after the rash fades. That means you could be spreading the virus while feeling perfectly fine—something the CDC emphasizes in its 2025 rubella factsheet.
Because the virus travels so easily, unvaccinated children, travelers returning from regions where rubella is still common, and adults who missed their childhood shots become the primary sources of new cases in countries where the disease is “eliminated.”
Want to see how rubella stacks up against another respiratory foe? Check out this quick comparison with whooping cough and notice the similar ways both illnesses spread.
Who’s Most at Risk?
- Unvaccinated individuals: especially school‑age children and adults without documented immunity.
- International travelers: rubella still circulates in many parts of Asia, Africa, and South America.
- Women of child‑bearing age: if they haven’t been immunized, a single exposure can have serious consequences for a future pregnancy.
Silent carriers
About 25‑50 % of infected people never develop a rash or fever, yet they can still transmit the virus. That’s why health officials recommend a simple blood test (IgG antibody) to confirm immunity before planning a pregnancy. It’s quick, painless, and can spare you a lot of worry later.
Pregnancy Risks
Now, let’s get to the heart of the matter. If you’re pregnant—or thinking about it—rubella becomes more than a fleeting rash; it’s a potential threat to the developing baby.
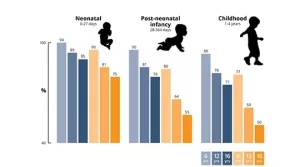
The virus crosses the placenta and can interfere with organ formation, especially during the first 12 weeks. According to the CDC, infection during this window carries a roughly 25 % chance of causing Congenital Rubella Syndrome (CRS). The risk drops dramatically after week 20, but it’s never zero.
What is CRS?
CRS is a collection of birth defects that can include:
- Blindness or cataracts
- Deafness
- Heart defects (especially patent ductus arteriosus)
- Microcephaly and brain damage
- Intellectual disability
These problems aren’t just medical footnotes—they affect a child’s entire life trajectory. Imagine preparing for a newborn’s first smile only to learn that a preventable virus could have altered that future.
Trimester‑by‑trimester risk table
| Trimester | Typical Fetal Impact | Common Outcomes |
|---|---|---|
| 0‑8 weeks | Severe organ malformation | Cataracts, heart defects, hearing loss |
| 8‑12 weeks | High CRS risk | Deafness, brain anomalies, growth restriction |
| 13‑20 weeks | Moderate CRS risk | Minor heart issues, possible vision problems |
| >20 weeks | Low CRS risk (but still possible) | Occasional hearing loss or mild developmental delays |
If you’re planning a family, a simple blood test can tell you whether you already have immunity. If not, the CDC recommends getting the MMR vaccine at least four weeks before conception. It’s a small step that protects a whole future.
Real‑world story
My friend Maya thought she was low‑risk because she grew up in the U.S. and never had a “big” illness. A routine check‑up revealed she was not immune to rubella. She postponed her pregnancy plan for three months, got the MMR shot, and later welcomed a healthy baby boy. Maya says the peace of mind was worth every waiting day.
Other Complications
Rubella isn’t just a pregnancy concern. For the broader population, it can still cause uncomfortable—but usually non‑life‑threatening—issues.
Arthritis in adults
Up to 70 % of adult women who contract rubella experience joint pain that can linger for weeks or months. It’s rarely severe, but it does add an extra layer of “ouch” to an otherwise mild illness.
Rare neurological events
In immunocompromised individuals, rubella can lead to encephalitis (brain inflammation) or thrombocytopenia (low platelet count). These complications are uncommon—occurring in less than 1 % of cases—but they underline why vaccination remains the safest route.
Case study snippet
A 2023 case report from the CDC described a teenager with an undiagnosed immune deficiency who developed encephalitis after a seemingly mild rubella infection. The patient recovered fully after intensive care, yet the episode serves as a reminder that even “mild” viruses can act up in vulnerable bodies.
Link to other vaccine‑preventable diseases
If you’re curious how rubella’s risk profile compares to other viral illnesses, take a look at measles risks. Both share a similar transmission route, but rubella’s real danger shines brightest during pregnancy.
Prevention Tips
The good news? Rubella is one of the most preventable viral infections on the planet. All you need is the MMR (measles‑mumps‑rubella) vaccine—or the combined MMRV (adds varicella). Let’s break down the what, why, and how.
MMR vaccine basics
- Efficacy: Over 97 % develop protective antibodies after two doses.
- Safety: It’s a live‑attenuated vaccine—meaning the virus is weakened, not active. It’s safe for kids over 12 months and adults, but NOT for pregnant people.
- Schedule: First dose at 12‑15 months, second dose at 4‑6 years. If you missed a dose, a catch‑up series is easy.
For those wondering about the vaccine benefits beyond rubella, the MMR also shields you from measles and mumps—both of which can cause serious complications on their own.
Quick FAQ for the MMR
- Can I get MMR while pregnant? No. Wait until after delivery (usually six weeks postpartum).
- Do adults need a booster? Only if you can’t confirm immunity with a blood test.
- What if a family member is allergic to eggs? The MMR vaccine contains no egg protein, so it’s safe for most egg‑allergic individuals.
Steps for non‑vaccinated people
- Schedule a rubella IgG test with your doctor.
- If non‑immune, arrange the MMR series well before any pregnancy plans.
- Practice good hygiene during outbreaks—regular hand washing, avoid close contact with symptomatic individuals.
- Encourage friends and family to stay up‑to‑date on vaccinations; herd immunity protects the most vulnerable.
Checklist (print‑friendly)
☑️ Verify immunity (blood test)
☑️ Get MMR if needed
☑️ Keep vaccination record accessible
☑️ Share accurate info with loved ones (like this article!)
Putting It All Together
Rubella may feel like “just a rash,” but its dangers become glaring when you consider the potential impact on a developing baby, the occasional joint pain in adults, and the rare but serious neurological complications. The best defense—vaccination—has already turned rubella from a common childhood illness into a rarity in many high‑income countries.
If you’re in a situation where you’re unsure about your rubella immunity, take a moment today to schedule that blood test. If you’re already immune, great—keep that record handy and encourage the people around you to stay current on their shots.
Remember, protecting yourself isn’t just about avoiding a sore throat; it’s about safeguarding future generations, preserving the joy of an uncomplicated pregnancy, and keeping the ripple effect of disease‑free families alive.
Take Action
Feeling ready to check your immunity? Talk to your healthcare provider, ask for a rubella IgG test, and if needed, line up that MMR vaccine. If you have questions about how vaccination fits into your overall health plan, explore more about vaccination importance. And if you know someone who’s planning a family, share this article—knowledge is the most generous gift you can give.
What’s the biggest takeaway for you? Let’s keep the conversation going. If you’ve ever faced a rubella scare or have tips on staying vaccine‑up‑to‑date, feel free to reach out. We’re all in this together, and together we can keep rubella dangers firmly in the past.





















Leave a Reply
You must be logged in to post a comment.