This isn’t just another cold in the daycare.
You’re probably thinking, “Whooping cough? Isn’t that some old-school disease?”
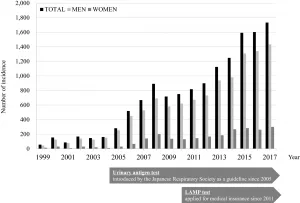
You wouldn’t be alone. But here’s the kicker: cases in Western Australia have jumped by 30% this year. And guess who’s getting crushed? Babies. Infants. Newborns. The ones who can’t speak up for themselves. One mom lost her child to pertussis. Now she’s rallying parents to vaccinate. Are people listening? Not really. And that’s the problem.
So, Who (or What) is Responsible For This?
Let’s break it down—why WA is seeing a spike
Whooping cough doesn’t play fair.
It slinks in like a common cold. Sniffles. Moody coughing. Then BAM—violent, unrelenting coughing fits. And here’s where it gets messy: vaccination rates in WA are dipping. A 2025 report from the state health department blames “vaccine hesitation” and “overlooked boosters.” Maybe parents are booking pedi appointments for sports check-ups but skipping the shots. Maybe adults assume they’re immune because they had the bug in 9th grade.
Whatever the reason—babies are paying the price. Data shows they’re at 68% risk for apnea, 22% for pneumonia, and 1 in 100 might not survive. That’s not a risk you can shake off with “we’ll be fine” vibes.
How are babies the biggest victims?
Here’s the brutal truth: infants under six months can’t defend themselves. They haven’t finished their DTaP shots (2, 4, 6, 15-18, and 4-6 years). Without full protection, they’re pancake-flat on immunity.
Australia’s CDC-style agency found that over half of infected babies end up in hospitals. Why? Because when a newborn starts gasping for air, or their lips turn blue after a coughing jag—it’s game over for pretending.
One case study had me gripping my seat: a 10-week-old spent 17 days on oxygen support. Parents thought it was “allergies” until the child flat-out stopped breathing.
What’s Going On With the Symptoms? Let’s Decode This Cough
You might think: “How’s this different from a cold?”
Great question.
Early symptoms of whooping cough are sneaky. Runny nose. Mild fever. Cough that seems “eh, whatever.” But here’s where it goes sideways: after 1-2 weeks, the cough evolves. It’s no longer a casual throat-clear. It’s a brutal fit that rips air from your lungs, ends with a “whoop” because you’re desperate to breathe, and—yeah—it can make you puke. Kinda romantic, right?
For adults? It might feel like a hungover cold. But for babies? As the CDC explains, one in three hospitalized infants has complications like pneumonia or seizures. Scary numbers—because babies don’t cough. They stop breathing.
But what happens if your child doesn’t ‘whoop’?
You’re not losing your mind. Whooping is… optional. Like the “whoop” is the encore, not the main event. The Cleveland Clinic notes some kids just get apnea or low-grade fever. No warning signs. No whoop. Just sudden silence. That’s when you hit panic mode and call the doctor.
A pediatrician in Perth told me about a 4-month-old who came in with “mild cough” for five days. By day six, she’d stopped breathing twice at night. Moral of the story: don’t wait for the whoop.
Adults: when it’s not just a bad flu
Plenty of adults shake off the vaccine. “I’ll fight it myself.” Except among parents of infected babies, 60% caught it from unvaccinated adults. A friend’s cousin had to literally wear a rib belt for cracked bones after coughing sessions. Yeah, it’s that intense.
The AMA’s Dr. Kuban compares adult whooping cough to “your worst stomach flu minus the diarrhea.” You cough so hard, blood vessels burst in your eyes. You fight for sleep. And here’s the doozy: antibiotics only help if you start them within the first seven days of symptoms. After that? You’re just coughing through the pain.
Let’s Talk Vaccines—Yes, Again
Why you (yes, you) should get the shot—even if you swear you don’t need it
Vaccines aren’t magical forcefields. They’re the next best thing—since we can’t put a baby in bubble wrap forever. CDC guidelines (2024 edition) suggest DTaP for babies, Tdap for preteens, and adult boosters every decade.
The catch? Herd immunity dies when adults skip boosters. Here’s the real talk: one study in NFID found unvaccinated adults are 10x more likely to spread pertussis. And if you think “vaccine side effects” are a dealbreaker: 1% of people get a low-grade reaction. Not zero percent worse than suffocating a baby.
Debunking myths—no, the shot won’t make your kid…
My sister once whispered to me, “Did you know the vaccine causes autism?” I paused for exactly 2.4 seconds—then texted her links. Because here’s the cold, unsexy truth: nope. The WHO’s 2025 review explicitly states this. Forget the fear-mongers. Focus on the 100-day cough that’s 1 in 100 for babies.
“Cocooning” or “protect the helpless”
Here’s how smart families win: not just vaccinating the baby. The whole . damn . household. Doctors call it “cocooning,” but really, it’s basic love. Grandparents. Babysitters. Even that friend who insists they’re “not sick.” If your kid’s under six months, get them Tdap.
WA’s recent policies updated school nurse protocols—now they email reminders to families of newborns: “Check vaccination status for everyone in the home.” It works. A 2025 CDC chart shows cocoon strategies slashed infant hospitalizations by 44% in outbreak zones.
Treatment Reality Check—Why Your Instincts Might Fail
When antibiotics are silver bullets or … when they’re not
You’re feeling it: zipper-deep fatigue, lungs getting razed by coughing. Should you rush for antibiotics?
Short answer: If you’ve had symptoms under a week, antibiotics like Azithromycin can soften pertussis. But wait too long, and they’re for reducing contagion—not late treatment. The MedlinePlus guide nails it: taking medicine early is like heading home before a school night-out. Too long? You’re the one coughing through the morning coffee.
Why hospitals are your best bet—when you see these red flags
Let’s not sugarcoat it:
You can DIY the beginning of this. Humidifiers. Small meals. Lots of fluids. But once fits start wrecking ribs, landing blue around the lips, or your baby has a dream where they forget to breathe—you call the doctor live.
In hospitals, they’ll do airway suction, IV hydration, and maybe oxygen. Ever heard of a 9-month-old needing oxygen just to sleepy-time? Neither have I. But doctors did. That’s why 30% of infected infants under six months require hospitalization, per Nemours KidsHealth.
Caregiver tips: what NOT to do when little lungs demand your patience
I get it. You’re panicking. But forcing honey down a baby’s throat? Huge mistake. MedlinePlus warns honey can cause botulism for kids under one. And over-the-counter cough syrup? Mic drop—they don’t work on bacterial coughs. Pertussis hackathon? No shortcuts.
Stick to what you can control: quarantine. Antibiotics for exposed family. And wash. those. hands. Hard. If you’re not in a red zone for pertussis—we’ve loosened hygiene standards. If you are? Gloria from the hospital will sort that between rounds of airway suctioning.
Prevention: Your Lifesaving Playbook
Vaccination schedules—the cheat sheet
The fight against whooping cough runs on a calendar. Here’s a table to save time, because you’ve got an infant to protect and it’s real life stuff. Leafing through health pamphlets isn’t your jam.
| Age | Vaccine Name | Protection Goal |
|---|---|---|
| 2, 4, 6 months | DTaP | Build immunity in babies |
| 15-18 months + 4-6 years | DTaP add-ons | Strengthen defense |
| 11–18 years | Tdap | Boost fading immunity |
| Adults (19+) | Tdap booster | Prevent transmission |
| Pregnant parents | Tdap (third trimester) | Pass antibodies to baby |
Exposed? What to do (besides panic)
So your toddler’s daycare has two cases. Cool. You’ve got drills for fire, so you’ll apply the same here: at exposure, contact the doctor immediately. They might prescribe preventive antibiotics for the entire household—even if nobody’s coughing yet. Because whooping cough is contagious before symptoms hit. Sneaky, right?
Also? Deep-clean surfaces. The Centers for Disease Control say pertussis can linger on a phone screen for four hours. You turn red thinking about the crib handle teeming with germs.
Travel concerns—should you double-check the shot?
If you’re jetting to WA (pun intended), India, or Nigeria right now? Yes, check vaccine records. Most countries trach cases as part of immunization programs, but travel health clinics will flag pertussis as a risk during flu season peaks. The CDC’s global data shows outbursts in Asia, Africa, and even the U.S.—so for a family trip to Bali or a work trip to Sydney? No shame in updating your Tdap.
Final Thoughts: Protect What Matters
If you’re still thinking, “This won’t hit us,” let’s chat. Pertussis doesn’t care about your clean diet, your immune-boosting hacks, or your anti-cough syrup philosophy. It’s a bacterial toilet-trained to hitch rides on speckles in the air, on kitchen counters, on sneeze-prone caregivers. And it’s ruthless when it hits babies.
But here’s the hopeful part: vaccines work. Antibiotics help. Cleaning. Masking. Hygiene. It’s not glamorous. It’s not “natural healing.” But cures are for people who COME down with it. Prevention is for those of us who’ve got our arms around what matters.
If you’ve got a child under six weeks, walk your tired self over to the pediatrician. Got a case of “why are they wheezing?” text the clinic. Don’t sit in a Google spiral—where every article modifies your zoom level on mortality stats. Coughing is urgent, not a learning moment.
Baby?
You email the doctor about Tdap now. Partner?
Get that shot. Yourself?
Boosters every ten years—the closest thing to “set and forget.”
This isn’t about trusting an algorithm. It’s about protecting loud.
























Leave a Reply
You must be logged in to post a comment.