Hey there, friend. If you’re scrolling through endless lists of “what to eat” and feeling a little overwhelmed, you’re in the right spot. Below you’ll find four tasty, gut‑friendly meals that fit perfectly into any UC diet plan. No fancy sauces, no mystery ingredients—just straightforward, soothing dishes that won’t set off a flare‑up.
Why does this matter? Because the right ulcerative colitis recipes can give your gut a breather, keep essential nutrients flowing, and still feel like you’re treating yourself. Let’s dive in together, and I’ll share a few personal twists that have helped me (and a few friends) on rough days.
Understanding UC Basics
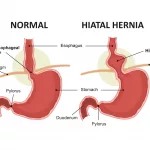
First, a quick reality check. Ulcerative colitis (UC) is an inflammatory condition that targets the lining of the colon. While everyone’s triggers differ, common culprits include high‑fiber foods, excess fat, dairy, and spices. A study in Gut (2023) showed that a low‑residue diet can lower daily stool frequency by up to 30 %.
But here’s the good news: food can also be your ally. Anti‑inflammatory ingredients—think turmeric, ginger, and omega‑3‑rich fish—help calm the fire inside. And when you pair those with low‑residue, easy‑to‑digest meals, you give your gut a chance to recover without sacrificing flavor.
What Triggers a Flare‑up?
Typical triggers include:
- High‑fiber raw vegetables (think broccoli stems, corn, and popcorn)
- Heavy, fried, or greasy foods
- Dairy for those who are lactose‑intolerant
- Spicy sauces and excess caffeine
Everyone is unique, so keeping a simple food‑symptom journal can pinpoint your personal troublemakers.
How Diet Calms Inflammation
Anti‑inflammatory foods work like a gentle fire‑extinguisher. Turmeric, for example, has been shown to be as effective as ibuprofen for reducing joint inflammation according to a clinical study. Pair it with a bit of healthy fat (olive oil) and black pepper, and your body absorbs the curcumin even better.
Key Nutrients You Might Miss
During flare‑ups, it’s easy to lose track of vitamins and minerals. Watch out for:
- Vitamin D (supports immune regulation)
- Vitamin B12 (helps red‑blood‑cell formation)
- Iron (to avoid anemia)
- Calcium (keeps bones strong without aggravating the gut)
Consider a quick chat with a dietitian if you suspect any gaps.
Core Cooking Principles
Low‑Residue, Gut‑Friendly Basics
Low‑residue meals limit undigested fiber, giving the colon a break. Safe staples include:
- Smooth pureed soups
- White rice, polenta, or refined pasta
- Well‑cooked carrots, zucchini, and peeled potatoes
- Lean proteins like chicken, fish, or tofu
Balancing Anti‑Inflammatory Foods
Every recipe below sneaks in at least one anti‑inflammatory hero—turmeric, ginger, or omega‑3 fats. These aren’t just for flavor; they actively help dampen the immune response that fuels UC.
Portion Control & Symptom Monitoring
Even the right food can cause issues if you overdo it. Aim for meals around 300‑500 kcal, and split larger plates into smaller, manageable portions. Note how you feel 2‑4 hours after eating—this is where your journal becomes a lifesaver.
When a Recipe Is “Too Risky”
If a dish feels too heavy, greasy, or packed with raw veggies, pause. Substitute:
- Swap whole‑grain pasta for white pasta
- Replace a whole‑milk sauce with a light coconut‑milk drizzle
- Leave out onions or garlic if they’re known triggers
Four Simple Recipes
Pumpkin Pancakes – Breakfast Comfort
Why I love them: they’re soft, slightly sweet, and packed with vitamin A. Perfect for a morning when your stomach is still saying “please be gentle.”
- Key ingredients: pumpkin puree, oat flour, cinnamon, a touch of maple syrup.
- Step‑by‑step:
- Whisk 1 cup oat flour with ½ tsp baking powder.
- Stir in ¾ cup pumpkin puree, ¼ cup milk (or dairy‑free alternative), 1 tbsp maple syrup, and a pinch of cinnamon.
- Heat a non‑stick pan, lightly oil, and pour batter (≈¼ cup per pancake).
- Cook 2‑3 minutes each side until golden.
- Serve warm, maybe with a dollop of lactose‑free yogurt.
Nutrition snapshot: ~260 kcal, 9 g protein, 2 g fiber (low‑residue). If you want a visual guide, check out a WebMD pumpkin pancake video for a quick walkthrough.
Turmeric Thai Curry – Lunch Power‑Boost
Picture a gentle, golden broth that smells like a spa day—that’s what turmeric does. This curry keeps the fat modest (half the usual coconut milk) while delivering a serious anti‑inflammatory punch.
- Key ingredients: chicken breast, sweet potatoes, turmeric, ginger, low‑fat dairy‑free milk, Thai curry paste.
- Custom swaps: use shrimp or firm tofu for a plant‑based version.
- Cooking steps:
- Dice 2 sweet potatoes and a chicken breast; set aside.
- Sauté 2 tbsp olive oil, 1 tbsp ginger (finely chopped), and 2 tbsp Thai curry paste for 1 minute.
- Add ½ cup coconut milk + ½ cup dairy‑free milk; stir.
- Drop in the sweet potatoes, simmer 15 minutes.
- Add chicken, cook until opaque (≈8 minutes).
- Finish with 1 tsp ground turmeric, a pinch of black pepper, and a splash of lime.
Nutrition per serving: ~327 kcal, 26 g protein, 3.8 g fat. A study notes that turmeric’s active compound, curcumin, can reduce gut inflammation when paired with fat and pepper—so this recipe is a science‑backed win.
Quinoa Power Bowl – Balanced Dinner
Quinoa is a complete protein, but if you find it a bit gritty, swapping for white rice is fine. The bowl is fully customizable—think of it as a canvas for whatever you have on hand.
- Key ingredients: 1 cup cooked quinoa, olive oil, rice vinegar, avocado, sun‑dried tomatoes, cucumber, feta (optional).
- Assembly:
- Mix cooked quinoa with 2 tbsp rice vinegar, 1 tbsp olive oil, salt & pepper.
- Layer diced avocado, cucumber, sun‑dried tomatoes, and crumbled feta on top.
- Garnish with fresh parsley and a drizzle of olive oil.
Nutrition snapshot: ~310 kcal, 8 g protein, 5 g fiber (still low‑residue). For a deeper dive into quinoa’s digestibility, see the InflammatoryBowelDisease.net guide.
Healing Carrot‑Ginger Soup – Flare‑Day Comfort
When your stomach rebels, a smooth soup is like a lullaby. This recipe uses bone broth for gut‑soothing gelatin, plus ginger for nausea relief.
- Key ingredients: carrots, onion, garlic, fresh ginger, chicken bone broth, coconut milk, olive oil.
- Steps:
- Sauté 1 tbsp olive oil with diced onion & minced garlic for 3‑5 minutes.
- Add half the sliced carrots; cook 10 minutes.
- Pour in 3 cups bone broth, 1 tsp ginger, and the remaining carrots; bring to boil.
- Simmer 30‑40 minutes until carrots are tender.
- Stir in 1 can coconut milk, then blend until silky.
Each bowl delivers ~250 kcal, comforting warmth, and a gut‑friendly nutrient mix. Freeze extra portions for “emergency” meals—just reheat and enjoy.
Customizing Your Plan
Low‑Residue vs. Higher‑Fiber Days
Some days you may crave fiber. The trick is to keep a “low‑residue” day before a potential flare and a “higher‑fiber” day when you’re feeling steady. Swap quinoa for white rice, or add a small side of peeled, steamed carrots to the power bowl.
Allergy or Intolerance Swaps
Allergic to dairy? Use lactose‑free cheese or a sprinkle of nutritional yeast. Gluten‑sensitive? All the recipes above work with rice‑flour pasta or gluten‑free noodles. The goal is to keep the base flavors while removing the trigger.
Scaling for Meal‑Prep
All four dishes freeze well. Double the pancake batter, portion into freezer bags, and toast later. The curry and soup become richer after a night in the fridge—so make a big batch on Sunday, label with dates, and you’ll have gut‑friendly meals ready all week.
Adding Probiotic Boosters
If your gut tolerates them, a side of plain kefir or a spoonful of fermented miso can introduce helpful bacteria. Just watch for added sugars, which sometimes cause irritation.
Safety Checklist Guide
Red‑Flag Symptoms After Eating
If you notice any of the following within a few hours, pause the recipe and consult your provider:
- Severe abdominal cramps
- Blood in stool
- Persistent vomiting or diarrhea lasting more than 24 hours
- Fever or unexplained weight loss
Tracking the Impact of Each Recipe
Use a simple table (feel free to copy‑paste into your notes) to log what you ate, portion size, and how you felt afterward. Over time, patterns emerge, and you’ll know which ulcerative colitis recipes are your go‑to comfort foods.
| Date | Meal | Portion | Symptoms (0‑5) | Notes |
|---|---|---|---|---|
| 2025‑08‑01 | Pumpkin Pancakes | 2 pancakes | 1 | Easy digestion, mild fullness |
| 2025‑08‑03 | Turmeric Curry | 1 cup | 0 | Great flavor, no cramps |
When to Call a Registered Dietitian
Consider professional guidance if you experience any of these:
- Unintended weight loss > 5 % in a month
- Persistent anemia or vitamin deficiencies
- Frequent flares despite dietary adjustments
- Complex food intolerances requiring detailed meal planning
Trusted Sources for Further Reading
For deeper dives, check out reputable sites like Healthline’s UC dinner ideas or the WebMD UC guide. They keep the information up‑to‑date and backed by clinicians.
Final Takeaway Summary
Living with ulcerative colitis doesn’t mean you have to surrender flavor or enjoy endless gray meals. The four recipes above—Pumpkin Pancakes, Turmeric Thai Curry, Quinoa Power Bowl, and Healing Carrot‑Ginger Soup—show that you can nourish your body, calm inflammation, and still savor every bite. Remember to listen to your gut, keep a simple symptom log, and adjust portions based on how you feel.
What’s your favorite gut‑friendly comfort food? Have you tried any of these recipes, or do you have a secret tweak that works for you? Drop a comment below, share your story, or ask any questions you might have. We’re all in this together, and every small, tasty step counts toward a calmer, healthier tomorrow.






















Leave a Reply
You must be logged in to post a comment.