Ever have those days where something just feels… off? Like, you wake up and there’s this weird tingling—like your foot fell asleep, but it’s not going away. At first, you try to shake it off (literally), maybe chalk it up to a bad night’s sleep. But then it lingers. And that’s when your mind starts spinning: “Wait, is this normal? Am I just imagining it? Or is my body trying to tell me something?”
First off—if you’re here, you’re not alone. The world of autoimmune small fiber neuropathy (yeah, it’s a mouthful!) can be confusing, even a little scary. But you don’t have to face it in the dark. Let’s walk through this together, with real talk, warmth, and maybe even a little hope.
So let’s dig in. We’ll get into what this “pins-and-needles” business is all about, why it happens (especially if you’ve danced the hard dance with autoimmune stuff or cancer treatment), and what you can actually do about it. Because you deserve answers—and, honestly, some peace of mind.
What Exactly Is Autoimmune Small Fiber Neuropathy?
Let’s keep it simple: autoimmune small fiber neuropathy is when your immune system (the body’s own defense squad) starts acting a bit… suspicious. Instead of just fighting off germs, it starts picking on your own tiny nerve fibers. These “small fibers” are the ones in charge of sending pain and temperature messages, plus helping with things like sweating and blood flow. When they get damaged, you end up with that persistent tingling, burning, or numbness—often in your hands and feet.
It’s like your nerves are trying to text your brain, but the messages are all jumbled up. Sometimes it’s just annoying. Other times, it feels downright unfair. And if you’ve already been through something tough—like cancer treatment or another autoimmune disease—it can feel like insult to injury.
How Do You Know If It’s This?
Great question. Early on, it might just feel like your foot’s asleep. But over time, the “pins-and-needles” can turn up the volume—burning, shooting pain, weird temperature changes, or even patches of numbness. It can sneak up slowly, or hit you all at once.
Some people notice it’s worse at night. Others say it feels like walking on gravel, even in cozy socks. If you’ve been through autoimmune disease after cancer treatment or have a history of myasthenia gravis, your risk goes up. But honestly, anyone can get it.
And if you’re nodding along, wondering, “Is this what’s happening to me?”—keep reading. You’re in the right place.
Why Does Autoimmune Small Fiber Neuropathy Happen?
Here’s where it gets wild: your immune system is supposed to be your best friend. But sometimes, after a big event (like an infection, or, yep, cancer treatment), it gets confused. Instead of just fighting off the bad guys, it starts going after your own nerves.
If you’re asking, “Is cancer an autoimmune disease?”—the answer is no, but cancer treatment can mess with your immune system in ways that make autoimmune issues more likely. It’s like your system is so revved up from the fight, it forgets where the real threat is.
Other things can set off this nerve drama, too. Genetics play a role (thanks, Mom and Dad?). And sometimes, it’s just bad luck—a perfect storm of immune confusion.
What About Other Autoimmune Diseases?
If you’ve already got something like rheumatoid arthritis (ever wondered about the diagnosis code for rheumatoid arthritis? It’s M06.9, by the way), myasthenia gravis, or Crohn’s disease, your immune system is already a bit quirky. It’s not that you’re “doomed,” but the odds of nerve issues like small fiber neuropathy do go up.
Think of your immune system as a watchdog. Sometimes, it barks at the neighbors (germs), and sometimes, it barks at the mailman (your own nerves). The trick is getting it to chill out—and that’s where proper diagnosis and treatment come in.
How Do You Get a Diagnosis?
Alright, so you’re feeling the weirdness. What now? First: don’t just Google and panic (though, hey, we’ve all done it). The real first step is talking to your doctor. And not just any doctor—a neurologist or rheumatologist who gets this stuff.
There’s no single test that screams, “Aha! It’s autoimmune small fiber neuropathy!” Instead, it’s a bit of a detective story. Your doctor might do:
- Skin biopsy: They take a teeny-tiny piece of skin (don’t worry, it’s quick) to look for nerve fiber loss.
- Nerve conduction studies: These check how well bigger nerves are working—if they’re normal, but you’ve got symptoms, small fiber neuropathy becomes more likely.
- Bloodwork: Looking for markers of autoimmune activity, vitamin deficiencies, or even infections.
- Special tests: Like the intrinsic factor antibody test (which checks for certain types of autoimmune trouble), or even genetic testing in rare cases.
And if your doc is really thorough, they’ll ask about your full medical history—like, “Hey, have you ever had myasthenia gravis or other weird autoimmune stuff?” Because all those puzzle pieces matter.
Personal Stories: Getting Answers Can Be a Journey
I once talked with someone who spent years bouncing between doctors, all while her feet felt like they were on fire. Test after test, everyone kept saying, “It’s just anxiety,” or, “Try these vitamins.” But she kept pushing. Finally, a neurologist did a skin biopsy and—bingo. Small fiber neuropathy.
Moral of the story? If you know something’s not right, trust yourself. Keep asking questions. You deserve answers.
Living With Autoimmune Small Fiber Neuropathy: Real Life, Real Challenges
Let’s get honest: living with this condition can be exhausting. Some days, it’s just background noise. Other days, it’s like your nerves are throwing a tantrum. But you’re not powerless.
Here’s what I’ve learned (and what others have shared with me): small changes can make a big difference.
- Rest and pacing: Listen to your body. Take breaks, even when you’d rather push through.
- Gentle exercise: Walking, swimming, yoga—movement can help, but don’t overdo it.
- Diet tweaks: Some folks notice certain foods make symptoms worse (hello, inflammation). Keep a food diary if you’re curious.
- Stress management: Easier said than done, right? But even a few minutes of deep breathing or meditation can help calm your nervous system.
And don’t forget the emotional side. It’s totally normal to feel frustrated, anxious, or even angry. Chronic pain is hard. If you need help, reach out—counseling or support groups can be a lifeline.
Balancing Benefits and Risks of Treatments
Okay, let’s talk about meds. There’s no one-size-fits-all fix, but there’s hope. Doctors might try things like:
- Pain relievers (sometimes prescription, sometimes over-the-counter)
- Medications to calm nerve pain—like gabapentin or duloxetine
- Immunosuppressants (to nudge your immune system back in line)
- IVIg (a fancy infusion that can help in some autoimmune cases)
Every treatment is a balancing act. The goal? To get your life back, without side effects stealing the show. Your doctor should walk you through the risks and benefits—and if they don’t, ask. You are your own best advocate.
And hey, it’s okay to try non-medication stuff, too—like physical therapy, acupuncture, or even therapy for your mental health. Sometimes it takes a whole team to get you feeling better.
Stories From the Frontlines
A friend with small fiber neuropathy told me her “aha” moment wasn’t a new medication, but finding a physical therapist who actually listened. They worked together on gentle stretches and nerve gliding exercises, and, little by little, the burning eased up.
It’s not a miracle cure, but it’s a reminder: everyone’s path is different, and sometimes the smallest changes make the biggest impact.
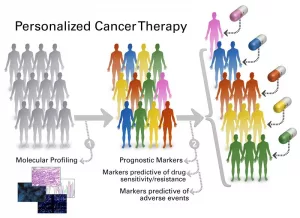
Treatment Options and New Advances—What’s On the Horizon?
Let’s get real—medicine is always evolving. Right now, doctors are experimenting with new treatments for myositis (another tricky autoimmune disease) that might help with nerve issues, too. There’s always research bubbling up, like immune therapies and even stem cell treatments.
Staying up-to-date can feel overwhelming, but it’s worth asking your doctor, “What’s new? What’s coming down the pipeline?” Because you deserve the best options, not just the old standbys.
And if you’re worried about insurance or disability, you’re not alone. People ask all the time: can you get life insurance if you have Crohn’s disease? Or, what about life insurance for multiple sclerosis, or can you get disability for sarcoidosis? The truth is, it can be tricky—but not impossible. Every company and policy is different, so shop around and don’t give up. Sometimes, sharing your doctor’s notes or showing stable treatment can help.
Comparing Related Autoimmune Conditions (Quick Table)
| Condition | Main Symptoms | Diagnosis Clues | Insurance Considerations |
|---|---|---|---|
| Autoimmune Small Fiber Neuropathy | Pins-and-needles, burning, numbness | Skin biopsy, nerve tests | Variable, depends on complications |
| Rheumatoid Arthritis | Joint pain, swelling, stiffness | Diagnosis code M06.9, blood tests | Can affect disability claims |
| Myasthenia Gravis | Muscle weakness, fatigue | History, specific antibody tests | May impact some coverage |
| Crohn’s Disease | Digestive issues, weight loss | Scans, endoscopy, history | Life insurance possible, needs proof of control |
| Sarcoidosis | Lung issues, fatigue, pain | Imaging, biopsy | Disability possible if severe |
If you recognize yourself in more than one of these rows—welcome to the club nobody asked to join! But also, know that you’re in good company, and there are resources and people who get it.
Moving Forward: Hope, Advocacy, and Real Connection
It’s easy to feel invisible when you’re dealing with something as sneaky as autoimmune small fiber neuropathy. Pain that doesn’t show up on the outside, doctors who don’t always understand, friends who just say, “You look fine!”—it can get lonely.
But here’s the thing: your experience is real, and your story matters. Whether you’re just starting to ask questions, or you’ve been fighting this battle for years, you’re not alone.
The best advice I can give? Stay curious. Keep asking, keep learning, and don’t be afraid to push for second opinions or new therapies. Medicine is changing all the time—sometimes the answer is just around the next corner. And if you ever feel like giving up, remember: small steps are still progress. Rest when you need to. Celebrate the good days. And reach out to people who get it—online, in support groups, or even right here in the comments.
Conclusion: You’re Not Alone—And You Deserve Answers
If you’ve made it this far—thank you. Seriously. It takes courage to dig into tough topics, and even more courage to keep searching for answers when you’re not feeling your best.
Remember: autoimmune small fiber neuropathy isn’t just a medical label. It’s something you’re living with, day in and day out. And while it might feel overwhelming, you’re stronger (and smarter) than you think. There’s no shame in asking for help, in demanding better care, or in taking time to rest.
If you have tips, stories, or questions—share them! You never know whose day you might brighten. And if you’re still searching for answers, keep going. Your story is worth telling, and hope is always part of the journey.
So, what do you think? Have you experienced these symptoms, or found something that helps? Drop a comment, start a conversation, and let’s keep supporting each other—one question, one story, and one small step at a time.





















Leave a Reply
You must be logged in to post a comment.