Hey there! If you’ve ever stared at a lab report and seen “mixed hyperlipidemia” and wondered what on earth that means, you’re not alone. Let’s cut through the jargon together, talk about why it matters, and explore what you can actually do about it—all in a friendly, down‑to‑earth chat. Grab a cup of tea, settle in, and let’s get started.
Quick Definition Explained
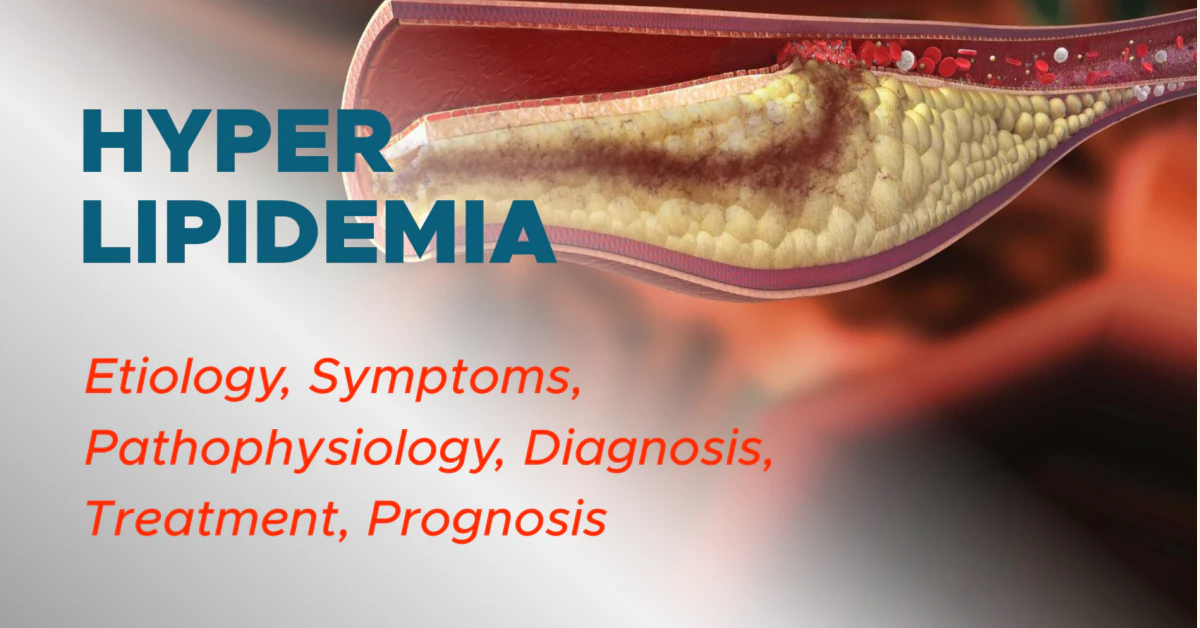
In plain language, mixed hyperlipidemia is a condition where two major types of “bad” fats in your blood are high at the same time: low‑density lipoprotein cholesterol (LDL‑C, the classic “bad” cholesterol) and triglycerides. At the same time, the “good” cholesterol (HDL‑C) is often low. Think of it as a traffic jam where both cars and trucks block the highway—your arteries get clogged faster.
Why the word “mixed”? Because it’s not just one lipid that’s out of balance; it’s a mixture of several, each contributing to the overall risk.
Prevalence & Genetics
Mixed hyperlipidemia is more common than you might think—about 1 % of the population, which translates to roughly 1 in 100 people. That makes it the most frequent inherited lipid disorder, according to Healthline and Healthgrades.
The condition often runs in families. If a parent has it, you have about a 50 % chance of inheriting the genetic predisposition. When both parents are affected, the risk can feel like a “double dose,” leading to higher lipid levels at a younger age.
But genetics isn’t destiny. Studies show that lifestyle factors (diet, activity, weight) can dramatically influence how the genes express themselves. In other words, your daily choices can tip the scales one way or the other.
Risk Factors Overview
Understanding who is most likely to develop mixed hyperlipidemia helps you stay ahead of the curve. Below are the major risk contributors, split into things you can’t change and things you absolutely can.
- Non‑modifiable: Family history, age (risk rises after 40), and certain ethnic backgrounds where the disorder is slightly more prevalent.
- Modifiable: A diet heavy in saturated fats and simple sugars, sedentary habits, excess body weight, heavy alcohol use, smoking, uncontrolled diabetes, and hypothyroidism.
Even subtle signs—like a faint ring around the cornea (arcus corneae) or tiny yellowish nodules on the skin (xanthomas)—can clue you in that something’s off. If any of these appear, it’s time to talk to a healthcare professional.
Diagnosis & ICD‑10
Diagnosing mixed hyperlipidemia starts with a fasting lipid panel. The key thresholds (as highlighted in BMJ’s “Investigating mixed hyperlipidaemia” paper) are:
- Triglycerides > 1.7 mmol/L (≈150 mg/dL)
- Total cholesterol > 5 mmol/L (≈190 mg/dL)
When both criteria are met, the clinician can label the pattern as mixed hyperlipidemia. The mixed hyperlipidemia ICD‑10 code is E78.01. This code helps providers bill correctly and ensures the condition is tracked in electronic health records.
Because other diseases can mimic or worsen the picture, doctors will usually run additional tests: thyroid function, liver enzymes, blood glucose, and sometimes a full metabolic panel. This way they rule out secondary causes like hypothyroidism or uncontrolled diabetes.
Health Impact Summary
Having both LDL‑C and triglycerides elevated is a double‑whammy for your heart and blood vessels. The excess fats embed themselves in arterial walls, accelerating atherosclerosis—the buildup that leads to heart attacks, strokes, and peripheral artery disease.
Research published in 2024 found that untreated mixed hyperlipidemia can shave 5–10 years off life expectancy, mainly because of earlier cardiovascular events. The good news? Early detection and aggressive management can bring that risk back down to the level of the general population.
Beyond heart disease, very high triglyceride levels (often > 500 mg/dL) raise the risk of acute pancreatitis, while chronic elevation contributes to non‑alcoholic fatty liver disease (NAFLD). So, the stakes are higher than a single cholesterol number.
Treatment Strategies Guide
There’s no magic cure, but there’s an excellent toolbox for keeping the numbers in check and protecting your heart.
First‑Line Lifestyle Changes
Think of lifestyle tweaks as the foundation of a house. If the foundation is solid, the rest holds up better.
- Diet: Aim for a Mediterranean‑style eating plan—lots of fruits, vegetables, whole grains, legumes, nuts, fish, and olive oil. Keep saturated fats below 7 % of total calories and cut out simple carbs (think sugary drinks, white bread).
- Exercise: At least 150 minutes of moderate‑intensity activity each week (brisk walking, cycling, swimming). Even short, 10‑minute bursts add up if you’re consistent.
- Weight Management: Losing just 5–10 % of body weight can lower triglycerides by up to 20 % and improve LDL‑C.
- Alcohol & Smoking: Limit alcohol to no more than one drink per day for women and two for men; quit smoking—your arteries will thank you instantly.
Pharmacologic Therapy
If lifestyle alone isn’t enough (which is often the case), medications step in. Below is a quick comparison of the most commonly used drug classes for mixed hyperlipidemia.
| Drug Class | Primary Goal | Typical Dose | Main Side‑Effects | When to Use |
|---|---|---|---|---|
| Statins | Lower LDL‑C | Atorvastatin 10–80 mg daily | Muscle aches, rare liver enzyme rise | First‑line for most patients |
| Fibrates | Lower Triglycerides | Fenofibrate 145 mg daily | GI upset, possible kidney issues | Triglycerides > 200 mg/dL, especially with high LDL‑C |
| Ezetimibe | Block cholesterol absorption | 10 mg daily | Diarrhea, mild liver changes | Added when statin alone isn’t enough |
| PCSK9 Inhibitors | Potent LDL‑C reduction | Injection every 2–4 weeks | Injection site reactions, flu‑like symptoms | High‑risk patients not reaching targets |
Many clinicians now start with a high‑intensity statin, then add a fibrate if triglycerides stay stubbornly high. Some patients benefit from a combo of statin + ezetimibe or even a PCSK9 inhibitor if their cardiovascular risk is extreme.
Clinical trial data suggests that combined statin‑fibrate therapy can reduce major cardiovascular events by up to 30 % compared with statin alone in mixed lipid disorders.
Monitoring & Goals
Targets may vary, but a good rule of thumb (according to the 2023 ACC/AHA lipid guidelines) is:
- LDL‑C < 100 mg/dL (or < 70 mg/dL if you've already had a heart attack or stroke)
- Triglycerides < 150 mg/dL
- HDL‑C > 40 mg/dL for men, > 50 mg/dL for women
After starting or adjusting therapy, re‑check your fasting lipid panel every 3–6 months until you hit those goals, then once a year.
Practical Takeaway Checklist
Let’s wrap everything up into a simple, actionable list you can keep on your fridge or in your phone notes.
Today’s Self‑Check
- Do you have a family history of high cholesterol or early heart attacks?
- Any visible xanthomas or a ring around the cornea?
- When was your last fasting lipid panel?
Lab Prep Guide
Next time you head to the lab, remember to fast for 12 hours, avoid alcohol the night before, and bring a list of any current medications or supplements. It makes the results more reliable.
Kick‑Start Lifestyle
- Swap one sugary drink a day for sparkling water with a slice of lemon.
- Walk during your lunch break—10 minutes is enough to start moving the needle.
- Try a weekly “meat‑free” dinner; plant proteins often come with lower saturated fat.
Medication Primer
If your doctor prescribes a statin, think of it as a “traffic police officer” for LDL‑C. If a fibrate joins the team, it’s the “clean‑up crew” for triglycerides. Together they keep the highway clear.
Long‑Term Outlook
Curious about how mixed hyperlipidemia might affect your years ahead? A detailed look at mixed hyperlipidemia life expectancy shows that with modern therapy, most people live as long and healthy as their peers without the condition.
Conclusion
So, what’s the mixed hyperlipidemia meaning in a nutshell? It’s a genetic‑plus‑lifestyle puzzle where both LDL‑C and triglycerides run high, raising your heart‑disease risk. The good news is that we have the knowledge, tools, and treatments to keep those numbers in check. By combining smart food choices, regular movement, and—when needed—targeted medication, you can protect your arteries and enjoy a vibrant, long life.
Remember, you’re not alone on this journey. Talk with your doctor about a lipid panel, ask about the what is mixed hyperlipidemia in the context of your family history, and take the first step toward a healthier future. If you’ve already wrestled with mixed hyperlipidemia, what strategies have worked best for you? Feel free to share your experiences—you might just help someone else feel less alone.























Leave a Reply
You must be logged in to post a comment.