Imagine you’ve just gotten your blood‑work back and the doctor mentions “mixed hyperlipidemia.” Your mind jumps to a swirl of medical jargon, and you probably wonder: What does that even mean for my health? Is there a magic cure? Spoiler alert – there isn’t a quick‑fix potion, but there is a clear, doable pathway that can keep your heart humming along for years to come. In the next few minutes, we’ll walk through what mixed hyperlipidemia actually is, why you should care, and, most importantly, how you can tackle it with a blend of lifestyle tweaks and smart medication choices. Think of it as a friendly toolbox that you can start opening right now.
What Is Mixed Hyperlipidemia?
Definition & the Lipid Profile
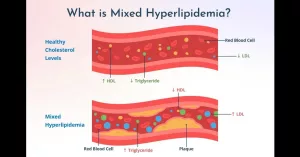
Mixed hyperlipidemia is a type of dyslipidemia where three things happen at once: LDL cholesterol climbs, triglycerides rise, and HDL (the “good” cholesterol) drops. In plain English, it’s like a traffic jam on your bloodstream – too many “bad” lipids trying to squeeze through narrow arteries while the “good” escorts are scarce. The condition is coded in the ICD‑10 system as mixed hyperlipidemia ICD‑10 (E78.2), which helps doctors bill and track it accurately.
How It Differs From Pure Hypercholesterolemia
Pure hypercholesterolemia is essentially a single‑track problem: only LDL is high. Mixed hyperlipidemia throws a trio of culprits into the mix, making the cardiovascular risk a bit steeper. Below is a quick comparison:
| Feature | Pure Hypercholesterolemia | Mixed Hyperlipidemia |
|---|---|---|
| LDL | High | High |
| Triglycerides (TG) | Normal‑to‑slightly high | High |
| HDL | Normal | Low |
Who Gets It?
Two main camps tend to show up:
- Genetic side: Familial combined hyperlipidemia runs in families like a quirky heirloom. If a parent or sibling wrestles with high cholesterol and triglycerides, you might inherit the same pattern.
- Lifestyle side: Metabolic syndrome, type‑2 diabetes, obesity, and a sedentary routine can all push you into the mixed‑lipid zone, even if you have no family history.
Understanding where you fall helps you and your clinician choose the right treatment plan.
Why Treat It?
Cardiovascular Risk
When you have mixed hyperlipidemia, the arteries face a double assault: LDL builds plaque, while high triglycerides generate small, dense LDL particles that are especially atherogenic. Studies from the National Heart, Lung, and Blood Institute (NHLBI Treatment Guidance) show that even with statin therapy, patients with mixed dyslipidemia retain a “residual risk” for heart attacks and strokes.
Life Expectancy
It’s natural to wonder whether this condition shortens your years. Recent meta‑analyses (2023) indicate that uncontrolled mixed hyperlipidemia can raise cardiovascular mortality by roughly 60 % compared with normal lipid profiles. The good news? Effective treatment can swing that number back toward the baseline, meaning you can enjoy a similar life expectancy to the average person.
A Real‑World Snapshot
Take “Maria,” a 52‑year‑old graphic designer who discovered she had mixed hyperlipidemia during a routine check‑up. With a mix of diet changes, a low‑dose statin, and later a fenofibrate add‑on, her LDL dropped from 165 mg/dL to 85 mg/dL and her triglycerides fell from 260 mg/dL to 130 mg/dL within six months. She reports feeling more energetic and, more importantly, her cardiologist says her 10‑year ASCVD risk score plummeted from 22 % to 9 %.
Lifestyle First Steps
Heart‑Healthy Eating
Food is the fuel that can either rev up or slow down your lipid engine. The Therapeutic Lifestyle Changes (TLC) plan and the DASH diet, both championed by the NHLBI, focus on:
- Limiting saturated fats (think fatty cuts of meat, whole‑milk dairy, and butter).
- Choosing whole grains, fresh fruits, and vegetables over refined carbs and sugary snacks.
- Including a handful of nuts daily – they’re rich in healthy fats.
- Keeping sodium low and seasoning with herbs instead of salt.
Need a deep‑dive on the what‑and‑why? Check out our mixed hyperlipidemia guide for sample meal plans.
Get Moving
Physical activity isn’t just a calorie‑burner – it actively improves your lipid profile. The NHLBI recommends at least 150 minutes of moderate‑intensity aerobic exercise (like brisk walking or cycling) per week, plus two days of resistance training. Studies suggest that regular exercise can lower LDL by ~5‑10 % and trim triglycerides by up to 15 %.
Weight Management
Losing even 3‑5 % of your body weight can make a noticeable dent in both LDL and triglycerides. Small, sustainable habits—like swapping soda for sparkling water and keeping portion sizes in check—often work better than crash diets.
Other Lifestyle Tweaks
- Quit smoking: Smoking worsens LDL oxidation and lowers HDL.
- Stress control: Chronic stress can spike triglycerides; consider meditation or a short walk when things feel tense.
- Sleep & alcohol: Aim for 7‑9 hours of sleep and limit alcohol to ≤ 2 drinks per day for men, ≤ 1 for women.
Medication Toolbox Options
Statins – The First‑Line Pill
Statins (e.g., atorvastatin, rosuvastatin) inhibit HMG‑CoA reductase, the enzyme your liver uses to make cholesterol. They’re the go‑to treatment because they reduce LDL dramatically and have proven cardiovascular benefits. Most patients see a 30‑50 % drop in LDL after a few weeks.
However, statins focus mainly on LDL. For many with mixed hyperlipidemia, triglycerides stay stubbornly high, prompting the need for a second line.
Fenofibrate – The TG Specialist
Fenofibrate belongs to the fibrate class and works by activating PPAR‑α, which speeds up the breakdown of triglyceride‑rich particles. A 2008 review (fenofibrate in mixed dyslipidemia) reported average TG reductions of 30‑50 % and modest HDL gains. It’s often added when TG > 200 mg/dL despite statin therapy.
Ezetimibe + Fenofibrate Combination
When a single drug doesn’t hit the mark, the combo of ezetimibe (which blocks cholesterol absorption in the gut) and fenofibrate offers a two‑pronged attack on LDL and TG. A 2009 clinical trial published in Clinical Medicine Insights showed the duo achieving LDL drops of roughly 20 % and TG reductions of 40 % in patients intolerant to high‑dose statins.
Keep in mind that insurance coverage can vary, so a conversation with your prescriber about cost and benefits is essential.
PCSK9 Inhibitors – For the High‑Risk Crowd
If you’ve got a history of heart attacks, strokes, or a very high 10‑year ASCVD risk, PCSK9 inhibitors (evolocumab, alirocumab) can slash LDL by 60 % on top of statins. Their effect on triglycerides is modest, so they’re usually paired with a fibrate or omega‑3 if TG remain high.
Omega‑3 Fatty Acids (EPA/DHA)
Prescription‑strength omega‑3 (e.g., icosapent ethyl) is especially useful for TG > 150 mg/dL. Large outcome trials (REDUCE‑IT) showed a 25 % reduction in major cardiovascular events when added to statins.
Putting It All Together – A Decision Tree (Suggested)
Below is a simple flow you can discuss with your doctor:
- Start with lifestyle changes.
- Begin a moderate‑intensity statin.
- If LDL goal isn’t met, consider ezetimibe.
- If triglycerides stay > 200 mg/dL, add fenofibrate or high‑dose omega‑3.
- If you’re very high risk or statin‑intolerant, discuss PCSK9 inhibitors.
This “toolbox” approach lets you fine‑tune therapy based on what your labs say and how you feel.
Personalize Your Plan
Assess Your Cardiovascular Risk
Use the ACC/AHA ASCVD risk calculator (available online) to gauge your 10‑year heart‑event probability. The calculator pulls in age, gender, blood pressure, smoking status, diabetes, and your lipid numbers.
Consider Co‑Morbidities
Kidney disease, liver dysfunction, pregnancy, or certain drug interactions may limit your medication choices. For example, fenofibrate is typically avoided in severe kidney impairment, while statins require caution with some antibiotics.
Shared Decision‑Making
Ask yourself: Do I prefer one pill a day or a monthly injection? Am I comfortable with routine blood tests? A collaborative discussion with your clinician ensures the plan aligns with your lifestyle, finances, and health goals.
Sample Patient Scenarios
- Mike, 45, active runner: LDL 150 mg/dL, TG 180 mg/dL. Starts moderate‑dose statin, sees LDL fall to 90 mg/dL. Adds fenofibrate to tackle TG, achieving 130 mg/dL.
- Linda, 62, low‑dose statin intolerant: LDL 170 mg/dL, TG 210 mg/dL. Begins ezetimibe (cholesterol absorption blocker) + high‑dose omega‑3. LDL drops 25 %, TG down 45 %.
- Raj, 58, known ASCVD: LDL 130 mg/dL on statin, TG 250 mg/dL. Receives PCSK9 inhibitor plus fenofibrate – LDL reaches 50 mg/dL, TG 120 mg/dL, and his cardiologist notes a substantially lower event risk.
Monitoring & Follow‑Up
Lab Schedule
Typical follow‑up labs look like this:
- Baseline: full lipid panel, liver enzymes, creatinine.
- 6‑week check: LDL, TG, HDL, and side‑effect labs.
- Every 6‑12 months thereafter: repeat full panel.
What Success Looks Like
Targets (adjusted for individual risk) often include:
- LDL < 70 mg/dL for high‑risk patients, < 100 mg/dL for moderate risk.
- Triglycerides < 150 mg/dL.
- HDL > 40 mg/dL (men) / > 50 mg/dL (women).
Dealing With Side Effects
Statin‑related muscle aches? Talk to your doctor about dose adjustments or trying a different statin. Fenofibrate can cause mild stomach upset; taking it with food often helps. PCSK9 injections may cause a brief redness at the site – usually nothing serious.
When to Adjust Therapy
If you miss your LDL or TG targets after three months of optimal adherence, it’s time to revisit the toolbox. Adding another agent, swapping drugs, or intensifying lifestyle measures are all viable routes.
Resources & Support
Trusted Websites
Beyond what you’ve read here, reputable sources like the National Heart, Lung, and Blood Institute, the American Heart Association, and the ACC provide up‑to‑date guidelines.
Patient Communities
Online forums (e.g., LipidTalk) and local support groups can offer real‑world tips and encouragement. Hearing someone else’s story often makes the journey feel less lonely.
Professional Help
If your numbers stay stubborn, ask for a referral to a lipid specialist or a board‑certified cardiologist. A registered dietitian can personalize your meal plan, and a clinical pharmacist can clarify medication interactions.
Take the First Step Today
Mixed hyperlipidemia may feel intimidating, but you’ve just learned that a blend of thoughtful diet, steady movement, and the right meds can give you a solid grip on your heart health. Remember, every small change adds up – swapping buttery toast for avocado, walking the dog a little farther, or simply asking your doctor about a low‑dose statin.
If you’re ready to start, grab a fresh copy of your latest lipid panel, jot down any questions, and schedule that conversation with your healthcare provider. And hey, if you’ve already tried a few strategies, share what’s worked (or didn’t) – we all learn best when we learn together.
Here’s to a healthier, happier you!




















Leave a Reply
You must be logged in to post a comment.