Hey there! If you’ve ever felt a firm little bump under the skin of your palm that didn’t hurt at all, you might be wondering, “Is that something I should worry about?” The answer could be yes — you could be looking at the first whisper of Dupuytren’s contracture symptoms. In this post I’ll walk you through what those early signs look like, how the condition can evolve, and what you can actually do about it—all in a friendly, down‑to‑earth style that feels more like a chat over coffee than a medical lecture.
Quick Symptom Checklist
Are there hard nodules or painless lumps on my palm?
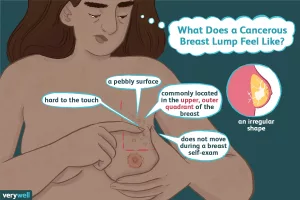
One of the most common Dupuytren’s signs is a small, firm nodule—often called a “painless lump”—that sits just under the skin, usually near the crease where your ring finger meets the palm. These nodules are typically ½ – 1 cm in diameter and feel hard, not squishy. They don’t usually hurt, which is why many people ignore them for months or even years.
What to feel for
- Size: roughly the tip of a pencil eraser.
- Location: under the 4th‑5th finger (ring‑little) crease.
- Texture: firm, almost like a tiny pebble.
Do I notice dimpling or ridges on the skin?
As the nodules mature, the skin on the palm can start to look a bit puckered or dimpled. You might even see a faint line or ridge that wasn’t there before. This is the hand’s way of saying, “Hey, something’s changing underneath.”
Visual cue
Take a quick photo of your palm opposite a plain background. A subtle indentation or a raised line that seems new? That could be the early rope‑like tissue forming.
Is a rope‑like cord pulling a finger inward?
When the condition moves from the “nodule” stage to the “cord” stage, you’ll feel a thin, rope‑like band under the skin. This cord can slowly tug one of your fingers—most often the ring or little finger—toward the palm. The finger may still straighten, but you’ll notice a slight resistance, especially when you try to flatten your hand.
Typical fingers involved
- Ring finger – the most frequent.
- Little finger – close second.
- Middle & index fingers – less common but possible.
- Thumb – rare, but it can happen.
Any itching, burning, or pressure sensations?
Even though Dupuytren’s contracture symptoms are often painless, a minority of people report a mild itching, burning, or a feeling of pressure around the nodule. According to the NHS, these sensations are not a sign of infection; they’re just the tissue reacting as it thickens.
How It Progresses
Stage 1 – Early (nodule) phase
At this point you have that solitary nodule, maybe a little dimpling. It’s usually painless, and many people never notice it until it grows. Some nodules even stay the same size forever, which is why the condition can be “quiet” for a long time.
Stage 2 – Active (cord) phase
Months to years later the fibrous tissue starts forming cords that connect the nodule to nearby fingers. The cords feel like a rubber band under the skin and may be visible as a thin line. This is when you might start feeling a gentle tug when you try to straighten the affected finger.
Stage 3 – Contracture (advanced) phase
Finally the cords tighten enough that the finger curls toward the palm and resists being flattened. This is the classic “finger contracture” many people think of when they hear the name Dupuytren’s. The tabletop test—trying to lay your palm flat on a table—fails, indicating a true contracture.
Quick staging table
| Stage | Key Signs | Typical Action |
|---|---|---|
| 1 – Nodule | Firm, painless lump under palm | Watchful waiting; hand‑therapy |
| 2 – Cord | Rope‑like band, mild finger pull | Injectable collagenase or steroids |
| 3 – Contracture | Finger stuck in flexed position | Surgery or needle aponeurotomy |
Other Hand Conditions
How is it different from trigger finger?
Trigger finger also creates a “catch” when you move the finger, but the problem sits at the tendon sheath, not under the palm. You’ll feel a popping sensation and the tip of the finger may lock, whereas Dupuytren’s shows a steady pull from the base of the palm.
How is it different from ganglion cysts or calluses?
Ganglion cysts are usually soft, fluid‑filled lumps that can move around a bit. Calluses are thickened skin that feels rough, not firm like a nodule. A quick press with your thumb usually tells the difference: firm nodules don’t squish.
When should a GP refer you to a hand specialist?
If you:
- Notice a nodule that’s growing.
- Feel a cord pulling a finger and you can’t fully flatten your hand.
- Experience functional loss—trouble gripping, washing, or buttoning.
Those red‑flags usually prompt a referral to a certified hand surgeon or a physiatrist who specializes in upper‑extremity disorders.
Getting a Diagnosis
The “table‑top test” – what it tells you
Place your palm flat on a table. If any part of the hand lifts off because a finger won’t straighten, that’s a positive tabletop test. It’s a quick, at‑home screen that tells you whether the contracture is already affecting your range of motion.
Physical exam – what the doctor feels for
A hand specialist will gently palpate your palm, looking for nodules, cords, and the degree of finger flexion. They’ll also measure the angle of each joint to track progression over time. According to MedlinePlus, this hands‑on exam is usually enough; imaging is rarely required unless the presentation is atypical.
Imaging & other tests (when are they needed?)
Ultrasound can map the thickness of the cords, and MRI is reserved for complex cases where surgery is being planned. Most patients never need these tests, but they’re handy tools when the surgeon wants a crystal‑clear roadmap.
Managing Symptoms
Non‑surgical options (early stage)
When you’re still in the nodule or cord stage, many people find relief without going under the knife.
Stretching & hand‑therapy
Gentle warm‑water soaks followed by finger‑extension stretches can keep the tissue from tightening too quickly. A simple routine—hold each stretch for 15 seconds, repeat three times a day—often stalls progression.
Injectable therapies
Collagenase (brand XIAFLEX) is an enzyme that “digests” the cords, allowing the doctor to break them apart manually. Studies quoted by eMedicineHealth show success rates of around 70 % for reducing contracture without surgery. Corticosteroid injections can also calm inflammation if the nodules are tender.
Lifestyle tweaks
Smoking, heavy alcohol use, and uncontrolled diabetes increase risk and can speed up progression. Cutting back on these factors isn’t a cure, but it can certainly keep the situation from spiraling.
Surgical options (advanced stage)
When a finger is truly stuck, the options move into the operating room.
Fasciectomy & needle aponeurotomy
Fasciectomy is the gold‑standard surgery: the surgeon removes the thickened fascia, freeing the finger. Needle aponeurotomy is a minimally invasive alternative where a needle slices the cord. Recovery for needle aponeurotomy is usually quicker (a few weeks of light activity) compared with the 6‑12 weeks of post‑fasciectomy rehab.
Post‑op rehab
Regardless of the procedure, hand‑therapist‑guided exercises are essential. They keep the new tissue flexible and prevent the cords from re‑forming. Expect daily stretching for the first month, then a gradual return to full activities.
Living With It
Hand‑care tricks to keep fingers functional
Even if you have a mild contracture, small adaptations can make daily life easier:
- Use ergonomic tools with larger handles (think “fat‑grip” pens or kitchen utensils).
- Wear a night‑time splint that holds the finger in extension while you sleep.
- Practice “palm‑flat” exercises each morning—place your hand on a flat surface and gently press to maintain full extension.
Monitoring progression at home
Take a monthly photo of your palm next to a ruler. Over time you’ll see whether the nodule is growing or the cord is lengthening. If you notice a sudden change, book an appointment sooner rather than later.
Myths vs. facts
Myth: “Heavy manual labor causes Dupuytren’s.” Fact: Repetitive hand work isn’t a proven cause; genetics and lifestyle factors dominate the risk profile. Myth: “If it’s painless, I don’t need a doctor.” Fact: Even painless nodules can become contractures that limit hand function, so early evaluation is wise.
Conclusion
Spotting Dupuytren’s contracture symptoms early can make a world of difference. A tiny, painless lump under your palm is often the first clue that your hand is beginning to remodel itself. By staying aware of nodules, dimpling, cords, and the occasional itch, you can decide when to watch, when to treat with injections or therapy, and when surgery becomes the best option.
Remember, you’re not alone in this. Many people walk the same path, and a supportive hand specialist can guide you through each stage with empathy and expertise. If any of the checklist items feel familiar, consider scheduling a quick exam—your future self will thank you for taking action now.
What’s your story? Have you noticed a nodule or experienced a finger that won’t straighten? Drop a comment below or share your experience with a friend who might be dealing with the same thing. Let’s keep the conversation going and help each other keep our hands strong and functional.






















Leave a Reply
You must be logged in to post a comment.