Most people don’t realize that Fanconi anemia is more than just a rare blood disorder. It’s a DNA‑repair problem that can cause bone‑marrow failure, birth‑defect anomalies, and a dramatically higher cancer risk. If you or someone you love has just been diagnosed, you’re probably looking for straight‑forward answers—what the disease looks like, why it happens, how it’s treated, and what the future might hold. Below, I’ve pulled together the most useful, up‑to‑date information in a friendly, “chat‑over‑coffee” style, so you can get the facts without wading through endless medical jargon.
What Is Fanconi Anemia
Definition
Fanconi anemia (FA) is a rare, inherited disorder that interferes with the body’s ability to repair DNA. Because the DNA‑repair pathway is broken, cells—especially those in the bone marrow—can’t make enough healthy blood cells. The condition is classified as an autosomal‑recessive DNA‑repair disease, though a few cases follow X‑linked or dominant patterns.
How Common Is It?
Statistics vary slightly by region, but researchers estimate that roughly 1 in 130,000 – 160,000 people are born with FA worldwide. That makes it rare enough to be “unknown” to many, yet common enough that dozens of families are coping with it every day.
Why the Name?
The syndrome is named after Dr. Guido Fanconi, who first described the characteristic bone‑marrow failure in the 1920s. Today, we honor his legacy by continuing to unravel the genetic secrets behind the disease.
Causes and Genetics
Genes Involved
More than 23 different genes can cause FA when both copies are mutated. The most famous are BRCA1 (known as FANCS) and BRCA2 (FANCD1), the same genes that drive many hereditary breast‑cancer families. Other common players include FANCA, FANCC, and FANCG. Each gene contributes a piece to the complex “FA pathway” that stitches broken DNA back together.
Inheritance Patterns
In most families, FA follows an autosomal‑recessive pattern: both parents carry one faulty copy of the same gene, and each child has a 25 % chance of inheriting both defective copies. A smaller subset of cases are X‑linked (usually involving the FANCB gene) or autosomal‑dominant, which slightly shifts the risk calculations. If you’re a carrier, genetic counseling can clarify your family’s odds.
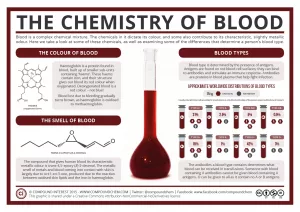
How Mutations Break DNA Repair
Think of DNA as a library of instructions. The FA proteins act like diligent librarians, spotting torn pages and repairing them before the information is lost. When the librarians are missing, errors pile up, leading to cell death, marrow failure, and the cancer‑prone environment that defines FA.
Quick Graphic Idea
If you were to illustrate this, you could draw a broken book (DNA) with a missing librarian (FA protein) and a chaotic pile of unread pages—a visual that helps friends without a science background grasp the concept.
Symptoms to Watch
Hematologic Signs
Because the bone marrow can’t keep up, people with FA often experience:
- Fatigue from anemia (low red blood cells)
- Frequent infections due to neutropenia (low white blood cells)
- Easy bruising or nosebleeds because of thrombocytopenia (low platelets)
These three “blood‑cell” problems are the classic Fanconi anemia symptoms that prompt a doctor’s visit.
Physical / Congenital Clues
FA is a multisystem disorder, so you might notice physical differences even before blood counts dip:
- Abnormal thumbs or missing radius bones (the forearm’s main bone)
- Short stature and a small head (micro‑cephaly)
- Café‑au‑lait spots or areas of light‑colored skin
- Kidney, heart, eye, or ear anomalies
- Skeletal curvature of the spine, hips, or ribs
These clues can be subtle, but together they often raise red flags for pediatricians.
When Do Symptoms Appear?
Most children are diagnosed between ages 3 and 14, yet about 10 % of cases aren’t discovered until adulthood—sometimes only after a cancer diagnosis. The age of onset can influence treatment decisions, so early recognition is key.
Case Vignette
Emily was seven when a routine school health check revealed low platelet counts. A quick physical exam showed a missing thumb on her right hand and a few café‑au‑lait patches on her arms. Those combined clues led her pediatrician to order genetic testing, confirming Fanconi anemia. Today, Emily is thriving thanks to a bone‑marrow transplant performed at age 12.
How It’s Diagnosed
Clinical Evaluation
Doctors start with a thorough physical exam and a detailed family history. Any combination of the congenital signs above, coupled with blood‑count abnormalities, warrants deeper investigation.
Laboratory Tests
A complete blood count (CBC) will reveal the trio of low red cells, white cells, and platelets. The gold‑standard “chromosome breakage test” (using diepoxybutane or mitomycin C) shows how fragile a patient’s DNA is—a hallmark of FA.
Genetic Testing
Next‑generation sequencing panels now screen all known FA genes in one go. Confirming the exact gene mutation helps predict disease severity and guides donor selection for transplant. According to the Fanconi Cancer Foundation, identifying the specific mutation also opens doors to emerging gene‑therapy trials.
Differential Diagnosis
FA can be confused with other bone‑marrow failure syndromes, like Diamond‑Blackfan anemia or severe aplastic anemia. The chromosome‑breakage assay and genetic results are the decisive factors that separate FA from these mimics.
Treatment Options
Supportive Care
While waiting for definitive therapy, many patients benefit from regular blood transfusions, iron chelation (to prevent iron overload), and growth factors such as G‑CSF (to boost white cells) or erythropoietin (to raise red cells). These measures improve quality of life but are not curative.
Androgen Therapy
Androgens like oxymetholone can stimulate marrow activity in some patients. Benefits are modest, and side‑effects (liver toxicity, hormonal changes) mean this isn’t a first‑line choice for most.
Hematopoietic Stem‑Cell Transplant (HSCT)
HSCT remains the only curative option for the blood‑cell problems of FA. Success rates have leapt from 30 % in the 1990s to over 80 % today when a well‑matched sibling donor is available. When a sibling isn’t an option, matched unrelated donor registries or haplo‑identical (half‑matched) transplants are increasingly successful.
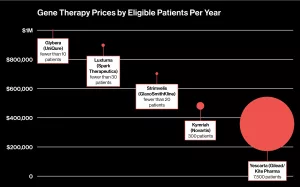
Emerging Therapies
Gene‑editing (CRISPR) and gene‑addition trials are in early phases, aiming to fix the underlying DNA‑repair defect. A handful of clinical studies (clinicaltrials.gov) are recruiting patients, offering a glimpse of a future where a simple infusion could replace a bone‑marrow transplant.
Managing Cancer Risk
Because FA dramatically raises the odds of acute myeloid leukemia (AML), head‑neck squamous‑cell carcinoma, and liver cancer, regular surveillance is non‑negotiable. This includes annual blood work, bone‑marrow exams, and age‑appropriate imaging (e.g., MRI for head‑neck screening).
Screening Schedule Table
| Age | Screening | Frequency |
|---|---|---|
| 0‑5 y | CBC, physical exam, renal ultrasound | Every 6 months |
| 6‑12 y | Chromosome breakage test, dental exam | Yearly |
| 13‑18 y | Bone‑marrow aspirate, MRI of head/neck | Every 12 months |
| 19‑30 y | Blood counts, liver ultrasound, colonoscopy | Every 12‑24 months |
| 31 y+ | Full oncology work‑up, endocrine panel | Every 12 months |
Prognosis and Outlook
Survival Trends
Life expectancy has more than doubled since the 1990s, thanks to better transplant protocols and vigilant cancer screening. Many patients now live well into their 40s and 50s, and a growing adult FA community enjoys active, productive lives.
Factors Influencing Prognosis
Key determinants include:
- Age at transplant – younger patients fare better.
- Specific gene mutation – some are associated with milder marrow failure.
- Presence of cancer – early detection improves outcomes.
- Access to specialized care – multidisciplinary FA centers make a measurable difference.
Quality‑of‑Life Considerations
Endocrine issues (like hypothyroidism or diabetes), fertility concerns, and psychosocial stress are common. Hormone replacement, fertility counseling, and mental‑health support are integral parts of comprehensive FA care.
Living With FA
Daily Health Tips
Here are a few friend‑to‑friend suggestions that help keep things manageable:
- Wash hands frequently; infections can spiral quickly.
- Stay hydrated and eat iron‑rich foods, but avoid excess supplements without a doctor’s order.
- Wear a medical alert bracelet that lists “Fanconi anemia – bone‑marrow failure risk.”
- Keep a symptom diary – noting fevers, bruises, or new skin spots helps your team act fast.
Family Planning & Genetic Counseling
If you’re thinking about having children, talk to a genetic counselor early. Options include pre‑implantation genetic testing (PGT) with IVF, prenatal carrier screening, or using donor gametes. Knowledge empowers you to make the best decision for your family.
Support Networks
Connecting with others who truly understand can lighten the emotional load. The Fanconi Cancer Foundation runs a patient‑registry, virtual tumor board, and peer‑support groups worldwide. Local rare‑disease organizations (like NORD) also list community resources and financial assistance programs.
Financial & Insurance Navigation
Medical bills can be daunting. Many FA families qualify for research grants, foundation scholarships, or Medicaid waivers. A social worker familiar with rare‑disease funding can help you map out a plan, so you can focus on health rather than paperwork.
Putting It All Together
Living with Fanconi anemia can feel like walking a tightrope—balancing blood‑cell counts, cancer surveillance, and everyday life. Yet the story is increasingly one of hope. Early diagnosis, modern stem‑cell transplants, and a growing toolbox of experimental therapies mean that many people with FA are now able to lead full, vibrant lives.
If you’re navigating this journey, remember you’re not alone. Reach out to specialists, join a community, and keep asking questions—your curiosity is a powerful ally. And if you’ve learned something useful, please share it with a friend who might need a gentle hand‑hold right now. Together, we can turn a rare diagnosis into a shared mission of resilience and knowledge.



















Leave a Reply
You must be logged in to post a comment.