Hey there! If you’ve ever wondered whether that occasional headache or a stressful week could be a tiny pre‑signal for something bigger down the line, you’re not alone. Women face a unique blend of biology, life events, and even medical biases that shape their future stroke risk in women. Below, I’m breaking it down in a friendly, chat‑like way—think of it as a coffee‑shop conversation with a health‑savvy friend.
Grab a cup, get comfy, and let’s dive into the three big things you should know to stay one step ahead of stroke. I promise to keep the medical jargon to a minimum and sprinkle in some real‑world stories so it feels less like a textbook and more like advice from someone who cares.
Why Women Are at Risk
What does “future” stroke risk really mean?
When we talk about future stroke risk, we’re looking at the probability of having a stroke sometime in the coming years—not just tomorrow, but over a decade or even a lifetime. Risk calculators (like CHA₂DS₂‑VA) use age, blood pressure, diabetes, and a few sex‑specific factors to estimate that likelihood. Think of it as a weather forecast for your blood vessels: it helps you bring an umbrella before the storm hits.
How do women’s numbers compare to men’s?
According to a UK Biobank analysis, women aged 18‑35 are about 44 % more likely to suffer an ischemic stroke than men the same age (Go Red for Women 2022 study). The gap narrows after 35, but women retain a slightly higher lifetime risk overall—roughly 4 % more than men, according to the Journal of Stroke review (2023).
Which biology makes the gap bigger?
Two main culprits: hormones and vessel size. Estrogen can protect arteries early in life, but fluctuations during pregnancy, menopause, or hormone therapy can destabilize that shield. Women also tend to have smaller cerebral arteries, which means a clot doesn’t need to be as big to block blood flow. These subtle differences add up over decades.
Does treatment bias matter?
Unfortunately, research shows that women with atrial fibrillation (AF) are often prescribed oral anticoagulants less frequently than men (Medical Xpress 2024). The result? Higher stroke severity and a missed chance for early prevention. Knowing this bias exists empowers you to ask the right questions at your next appointment.
Pregnancy‑Related Factors
How does a complicated pregnancy shape later risk?
Conditions like pre‑eclampsia, gestational hypertension, or gestational diabetes can cause lasting changes in your blood vessels—think of them as tiny, permanent roadworks on the highways of your brain. A study of over 10,000 women found that those with severe pregnancy complications had a 30‑40 % higher chance of a stroke later in life (Pregnancy complications stroke risk).
Is postpartum stroke a warning sign?
Post‑delivery, a woman’s body is a whirlwind of hormonal surges, blood‑clotting changes, and sleep deprivation. All of these can trigger a stroke, especially in the first six weeks after birth. If you’ve ever felt a sudden, severe headache or visual disturbance postpartum, don’t brush it off—seek care right away.
What about pregnancy‑related migraines or pre‑eclampsia?
Migraines that start or worsen during pregnancy often signal an underlying vascular sensitivity. Combine that with pre‑eclampsia’s high‑blood‑pressure spikes, and you’ve got a recipe for future stroke risk. Keeping a migraine diary and sharing it with your OB‑GYN can help catch patterns early.
Can a prior loss affect future risk?
Emerging data suggest that miscarriage or stillbirth may be linked to chronic inflammation, which can accelerate atherosclerosis. While the evidence isn’t yet definitive, it’s another reminder to discuss any pregnancy loss with your provider—not just for emotional support, but also for long‑term vascular health.
Hormonal Life‑Stage Changes
How does early menopause influence odds?
Women who hit menopause before 40 face a 1.5‑fold increased risk of ischemic stroke compared with those who transition between 50‑54 (American Heart Association 2021). Each year you postpone menopause reduces stroke risk by roughly 2 %—so the timing really matters.
Does hormone‑replacement therapy help or hurt?
The answer isn’t black‑and‑white. Some studies link combined estrogen‑progestin therapy to higher clot risk, especially if you start HRT more than a decade after menopause. Conversely, low‑dose estrogen started soon after menopause may preserve the vascular protection you lost. The key is personalized counseling—talk to a cardiologist and a gynecologist together.
What role do oral contraceptives play?
High‑dose estrogen pills, especially when paired with smoking, double the stroke risk in women under 35. Modern low‑dose formulations are safer, but if you’re a smoker or have hypertension, you might consider a progestin‑only method. It’s a quick conversation to have during your annual exam.
Can lifelong estrogen be protective?
A large Chinese biobank study found that greater cumulative estrogen exposure was associated with a lower risk of both ischemic and hemorrhagic stroke in postmenopausal women (Contemporary OBGYN 2023). In other words, a longer reproductive span—or carefully managed hormone therapy—might keep your arteries healthier longer.
Modifiable Risks for Women
Which traditional risks hit women hardest?
High blood pressure, diabetes, and high cholesterol remain the top three culprits. Yet women with these conditions often experience more severe strokes. That’s why diligent control of BP (target <130/80 mm Hg) and regular lipid panels are non‑negotiable.
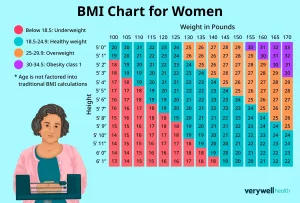
How does obesity affect women differently?
In the UCC‑SMART cohort, overweight women had a lower recurrence rate after an initial stroke—possibly because higher HDL cholesterol acted as a buffer (UCC‑SMART 2024). Still, excess weight raises the risk of hypertension and diabetes, so the overall advice stays: aim for a healthy BMI, but don’t obsess over the scale.
| Risk Factor | Impact on Women | Typical Intervention |
|---|---|---|
| Hypertension | 5‑year stroke risk ↑ 2‑fold | Lifestyle + ACE inhibitors |
| Diabetes | 3‑fold increase in ischemic stroke | Metformin, diet, HbA1c <7% |
| Smoking | 44 % higher stroke odds (18‑35 y) | Quit program, nicotine replacement |
| Obesity (BMI ≥ 30) | Higher recurrence if not overweight; overall risk ↑ | Balanced diet, regular activity |
Is smoking a bigger threat for young women?
Exactly. The combination of smoking and estrogen creates a pro‑coagulant environment. Young women who smoke and use combined oral contraceptives have up to a 5‑fold increase in stroke risk. Quitting even one cigarette a day can drop that risk substantially.
What lifestyle tweaks work best?
Here are five habits that pack the biggest punch:- Check your blood pressure at home—aim for under 120/80 mm Hg.
- Move your body: 150 minutes of moderate aerobic activity weekly (think brisk walks, dancing, or cycling).
- Adopt a DASH‑style diet rich in fruits, veggies, whole grains, and low‑fat dairy.
- Prioritize 7‑8 hours of sleep—sleep deprivation spikes blood pressure.
- Manage stress with mindfulness, yoga, or simply a weekly coffee chat with a friend.
Where can I find reliable risk tools?
The American Heart Association offers an online stroke risk calculator, and newer models like CHA₂DS₂‑VA specifically remove the “female” checkbox for AF patients, reflecting recent data that sex alone may not be enough (Medical Xpress 2024). Pick a tool that includes pregnancy history, menopause age, and hormonal therapy status for a truly personalized estimate.
ADVERTISEMENT
New Research & Tools
What’s new in risk scoring for women?
A 2024 Finnish FinACAF analysis suggested dropping the female sex point from the CHA₂DS₂‑VASc score because contemporary anticoagulation practices have narrowed the sex gap. The newer CHA₂DS₂‑VA still captures age, hypertension, diabetes, prior stroke, and vascular disease, but treats sex as a modifier, not a mandatory factor.
Do recent cohort studies change practice?
The Liverpool Centre’s 2024 paper showed that with better AF awareness and anticoagulant use, women’s stroke rates have fallen to near‑parity with men (Medical Xpress 2024). That’s encouraging, but it also means physicians can’t become complacent—ongoing vigilance is still essential.
Can genetics personalize risk?
Poly‑genic risk scores (PRS) are emerging tools that aggregate dozens of DNA variants linked to stroke. Early studies suggest that women with a high PRS and early menopause may benefit from more aggressive blood‑pressure control. While not yet routine, keep an eye on your doctor’s genetics clinic—they’re starting to offer PRS testing for at‑risk patients.
What gaps remain?
We still need:- Longitudinal data on hormone‑replacement therapy started at different ages.
- More diverse study populations—most large cohorts are predominantly White.
- Clear guidelines on integrating pregnancy complications into lifetime risk scores.
- Longitudinal data on hormone‑replacement therapy started at different ages.
- More diverse study populations—most large cohorts are predominantly White.
- Clear guidelines on integrating pregnancy complications into lifetime risk scores.
Until those answers arrive, the best strategy is to stay informed, ask questions, and keep a healthy lifestyle baseline.
Steps to Lower Your Risk
How should I talk to my doctor?
Prepare a one‑page “stroke risk sheet” before your visit. List:- Current meds (including birth‑control pills).
- Blood‑pressure readings from home.
- Any pregnancy complications you’ve had.
- Age at menopause or any HRT use.
Show the sheet, ask “Based on this, where do I stand on stroke risk?” and request a specific follow‑up plan.
Which screening tests are essential?
At a minimum, you should have:- Blood pressure check (in‑office and home).
- Lipid panel every 4‑6 years (more often if you have risk factors).
- Fasting glucose or HbA1c to rule out diabetes.
- Carotid ultrasound if you have a strong family history of stroke (Long‑term stroke risk).
- Hormone level assessment if you’re perimenopausal or on HRT.
What habits give the biggest reduction?
From the data, three actions shave off the most years of potential stroke risk:- Maintain a systolic BP <120 mm Hg.
- Quit smoking—risk drops by ~30 % within a year.
- Stay physically active—regular exercise cuts ischemic stroke risk by about 25 %.
When is medication indicated?
If you have atrial fibrillation, a CHA₂DS₂‑VA score of 2 or higher usually warrants an anticoagulant. For women with hypertension, a blood‑pressure‑lowering drug is recommended when lifestyle changes aren’t enough to get under 130/80 mm Hg. Always discuss side‑effects and adherence strategies with your clinician.
How can I stay updated on research?
Subscribe to reputable newsletters from the American Heart Association, Women’s Heart Foundation, or your local stroke association. Set a Google Alert for “future stroke risk in women” and you’ll get the latest studies straight to your inbox. And don’t forget to revisit trusted sites like maternal health and stroke for new insights on pregnancy‑related factors.
ADVERTISEMENT
Conclusion
- Maintain a systolic BP <120 mm Hg.
- Quit smoking—risk drops by ~30 % within a year.
- Stay physically active—regular exercise cuts ischemic stroke risk by about 25 %.
When is medication indicated?
If you have atrial fibrillation, a CHA₂DS₂‑VA score of 2 or higher usually warrants an anticoagulant. For women with hypertension, a blood‑pressure‑lowering drug is recommended when lifestyle changes aren’t enough to get under 130/80 mm Hg. Always discuss side‑effects and adherence strategies with your clinician.
How can I stay updated on research?
Subscribe to reputable newsletters from the American Heart Association, Women’s Heart Foundation, or your local stroke association. Set a Google Alert for “future stroke risk in women” and you’ll get the latest studies straight to your inbox. And don’t forget to revisit trusted sites like maternal health and stroke for new insights on pregnancy‑related factors.
Conclusion
Understanding the future stroke risk in women isn’t about living in fear; it’s about empowerment. From the hormonal twists of pregnancy and menopause to the everyday choices of diet, exercise, and medical communication, each piece of the puzzle can be shifted in your favor. By staying curious, asking the right questions, and embracing a heart‑healthy lifestyle, you give yourself the best chance to keep your brain thriving for decades to come. If you found any of this helpful, share it with a friend who might need a gentle nudge toward better stroke prevention. Here’s to a healthier, brighter future—together.





















Leave a Reply
You must be logged in to post a comment.