Quick answer: The Half‑Somersault Maneuver is a self‑administered head‑position exercise that re‑aligns displaced ear crystals in the posterior semicircular canal, providing fast relief from the spinning sensations of benign paroxysmal positional vertigo (BPPV).
Why BPPV
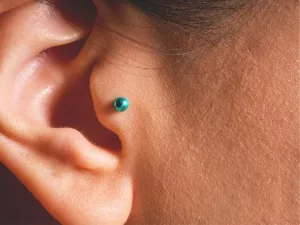
Ever woken up, swung your head to look at the ceiling, and felt the world start to spin like a lazy carousel? You’re not alone. BPPV is the most common cause of vertigo—affecting roughly half of all adults at some point in their lives. The culprit? Tiny calcium carbonate particles called otoconia that normally rest in the utricle of the inner ear. When they break free and tumble into a semicircular canal—most often the posterior canal—they confuse the brain’s balance sensors, sending a false “we’re turning” signal every time you change head position.
Typical triggers are mundane: rolling over in bed, looking up to grab a shelf, or getting out of a chair too quickly. The dizziness usually lasts only a few seconds to a minute, but during that brief window you might feel nauseous, unsteady, or even fear falling. If a simple “wait it out” approach isn’t cutting it, it’s time to consider a repositioning maneuver.
Science Behind
The Half‑Somersault Maneuver works on a straightforward principle: use gravity and a controlled head rotation to shepherd those rogue crystals back to their home in the utricle. Because the maneuver specifically targets the posterior canal, it’s most effective for the classic form of BPPV that doctors call “posterior‑canal BPPV.”
Clinical data backs it up. A 2021 comparative trial published in the Journal of International Advanced Otology reported that the Half‑Somersault showed similar success rates to the well‑known Epley maneuver while causing significantly less induced dizziness during the procedure. a 2021 study even highlighted its better tolerability—an important factor when you’re the one doing it at home.
Earlier, a 2012 randomized single‑blind study compared the two maneuvers over a six‑month follow‑up. While both reduced nystagmus (the involuntary eye movements that signal vertigo), the Half‑Somersault group experienced fewer treatment failures and reported a smoother recovery. the 2012 trial concluded that the half‑somersault is a viable, patient‑friendly alternative.
Bottom line: the maneuver is not a gimmick. It’s a well‑researched ear‑canal maneuver that moves otoconia using physics you can feel under your own fingertips.
Step‑by‑Step
Ready to give it a try? Grab a mat, clear a little space on the floor, and let’s walk through each movement together. Take it slow—the goal is precision, not speed.
1. Prepare the space
- Lay a yoga mat or a firm towel on the floor.
- Have a sturdy chair or a partner nearby for the first attempt, just in case you feel a wave of dizziness.
- Make sure you’re wearing comfortable clothing that won’t restrict movement.
2. Starting position
Kneel on the mat with your hands placed shoulder‑width apart, palms flat on the floor. Keep your chin lifted toward the ceiling as if you’re trying to touch the sky—this aligns your neck in a neutral position.
3. The “somersault” roll
Slowly bend your elbows to about 90°, then let your head tumble forward toward your knees. The back of your head should gently meet the mat, and your chin should tuck toward your chest. Imagine you’re starting a forward roll in gymnastics, but stop before your shoulders touch the floor. Hold this position for a breath (about 5‑10 seconds).
4. Side‑turn pause
Now, rotate your head toward the ear that’s affected. If you’re treating right‑side BPPV, turn your chin toward your right elbow; for left‑side, aim toward the left elbow. The goal is to get the ear perpendicular to the elbow, as if you’re pointing the “ear‑arrow” straight at it. Hold for 15 seconds—use a timer if you like.
5. Return to neutral
Bring your head back to the upright kneeling stance, still facing the same arm you just used. Hold for another 15 seconds, allowing any lingering dizziness to settle.
6. Sit up slowly
Finally, push yourself up to a seated position, keeping your head upright. Rest for at least 15 minutes before you consider repeating the sequence. If you feel better after the first round, you can stop; otherwise, repeat up to three times in the same session.
Modified versions for left vs. right
| Side | Head‑to‑Ceiling | Head‑to‑Mat | Side Turn | Hold Time (seconds) |
|---|---|---|---|---|
| Right | Look straight up | Back of head on mat | Chin toward right elbow | 15 |
| Left | Look straight up | Back of head on mat | Chin toward left elbow | 15 |
Feel free to print this table and keep it beside your mat—visual cues can make the routine feel less intimidating.
Benefits vs Risks
Every medical technique carries a balance of pros and cons, and the Half‑Somersault is no exception. Here’s a quick rundown so you can weigh the options consciously.
Benefits
- Effectiveness: Studies show ~80 % cure after a single session for many patients.
- Self‑administration: No need for a clinician to watch your eyes—ideal for home use.
- Comfort: Caused less immediate dizziness compared with the Epley maneuver in the 2021 trial.
- Time‑saving: Entire sequence takes under five minutes, plus resting time.
Risks & Contraindications
- Temporary nausea or mild headache during the roll.
- Transient nystagmus (eye‑jerking) may still occur.
- Not recommended for people with severe cervical spine issues, recent head trauma, or vestibular migraine without clear BPPV diagnosis.
- If dizziness persists beyond 24 hours after the maneuver, seek professional evaluation.
Minimizing Risks
Move deliberately, avoid jerky motions, and use a pillow under your head if you have a sensitive neck. If at any point you feel sharp pain, stop and rest—your body is giving you valuable feedback.
Full Rehab
Even after the crystals settle, many clinicians advise a broader vestibular rehab plan to keep the balance system strong and to reduce recurrence.
When to call a specialist
If you’ve tried the maneuver twice and dizziness is still a daily visitor, or if you notice unusual eye movements that don’t fit the classic BPPV pattern, it’s time to see an ENT specialist or a vestibular physical therapist. They can perform the Dix‑Hallpike test, video‑nystagmography, and tailor a personalized program.
Complementary exercises
- Brandt‑Daroff: Simple four‑position “rock‑the‑boat” movements that promote habituation.
- Semont (Quick‑turn) maneuver: Another repositioning technique for stubborn cases.
- Gaze stabilization drills: Focus on a fixed point while moving your head gently side‑to‑side.
Role of therapy
Physical therapists trained in vestibular rehab can teach you the correct posture, monitor your progress, and adjust exercises as you improve. Think of them as your balance coach—guiding you through the “practice” sessions so the brain learns to trust the new, correct signals.
Real‑World Stories
I remember meeting Sarah, a 38‑year‑old graphic designer who swore that vertigo had turned her work-from‑home days into a nightmare. She’d spent weeks avoiding the kitchen because the act of looking up to the fridge made her world spin. After a quick consult, she learned the Half‑Somersault from a vestibular therapist and practiced it nightly. Within a week, she reported that the dizzy spells were halved, and after three weeks she could finally stand up from her desk without a whirling sensation. “It felt like I finally got the cheat code for my inner ear,” she told me with a laugh.
Dr. Elena Morales, an ENT surgeon at a major university hospital, also champions the maneuver. She says, “I recommend the half‑somersault as a first‑line home exercise because patients find it less intimidating than the Epley. It’s a safe, effective option, especially for those with limited mobility.”
These anecdotes echo the data: the maneuver works, and it works in a way that feels achievable for everyday people.
Cheat Sheet
Below is a concise, printable reference you can keep on your nightstand. Just copy, paste into a Word document, and print!
| Step | Action | Hold Time |
|---|---|---|
| 1 | Kneel, hands shoulder‑width, chin up | 5‑10 s |
| 2 | Roll head forward, back of head to mat | 5‑10 s |
| 3 | Turn chin toward affected elbow | 15 s |
| 4 | Return to neutral kneeling | 15 s |
| 5 | Sit up slowly, rest | 15 min |
Conclusion
The Half‑Somersault Maneuver is more than a quirky name—it’s a scientifically validated, patient‑friendly BPPV treatment that you can safely perform at home. By understanding why vertigo happens, trusting the physics of the maneuver, and following a clear step‑by‑step guide, you empower yourself to reclaim daily life without the constant fear of a spinning world.
Remember, balance is a partnership between your inner ear, brain, and the actions you take. If the maneuver eases your symptoms, great! If not, don’t hesitate to reach out to a vestibular specialist—sometimes a professional eye on the problem makes all the difference.
Have you tried the Half‑Somersault? What was your experience? Share your story in the comments, ask questions, or let us know how you’ve integrated vestibular rehab into your routine. Together we can turn dizzy days into steady steps.





















Leave a Reply
You must be logged in to post a comment.