Hey there! If you’ve ever felt that dizzy swirl in your ear or struggled with sudden hearing drops, you’re probably wondering whether there’s a test that can actually “see” what’s going on inside. The short answer is yes—Endolymphatic Hydrops MRI does just that. In just a couple of minutes, this scan can reveal the hidden fluid imbalance that fuels Ménière’s disease, vestibular migraine, and a handful of other inner‑ear puzzles. Below, I’ll walk you through how it works, what the images mean, when you might need one, and the balance of benefits versus risks. Think of this as your friendly guide, not a medical textbook.
Why It Matters
Endolymphatic hydrops (EH) is the swelling of the fluid‑filled spaces inside the inner ear. When those tiny compartments get out of sync, you get vertigo, tinnitus, and fluctuating hearing loss. Until MRI entered the scene, doctors relied mostly on symptoms and audiograms—great, but not always definitive. Now, with a gadolinium‑enhanced scan, we can actually visualize the endolymph and perilymph compartments, giving us a concrete picture to base treatment decisions on.
Core MRI Techniques
| Technique | What It Shows | Typical Field Strength |
|---|---|---|
| Late‑enhanced 3D‑FLAIR (HYDROPS) | Contrast‑enhanced perilymph highlighting; endolymph appears dark | 1.5 T & 3 T |
| 3D‑CISS (Constructive Interference in Steady State) | High‑resolution anatomy of vestibular structures | 3 T preferred |
| Saccule‑Utricle Ratio Inversion (SURI) grading | Quantitative indicator of vestibular hydrops severity | Any high‑resolution scan |
Late‑enhanced 3D‑FLAIR (HYDROPS)
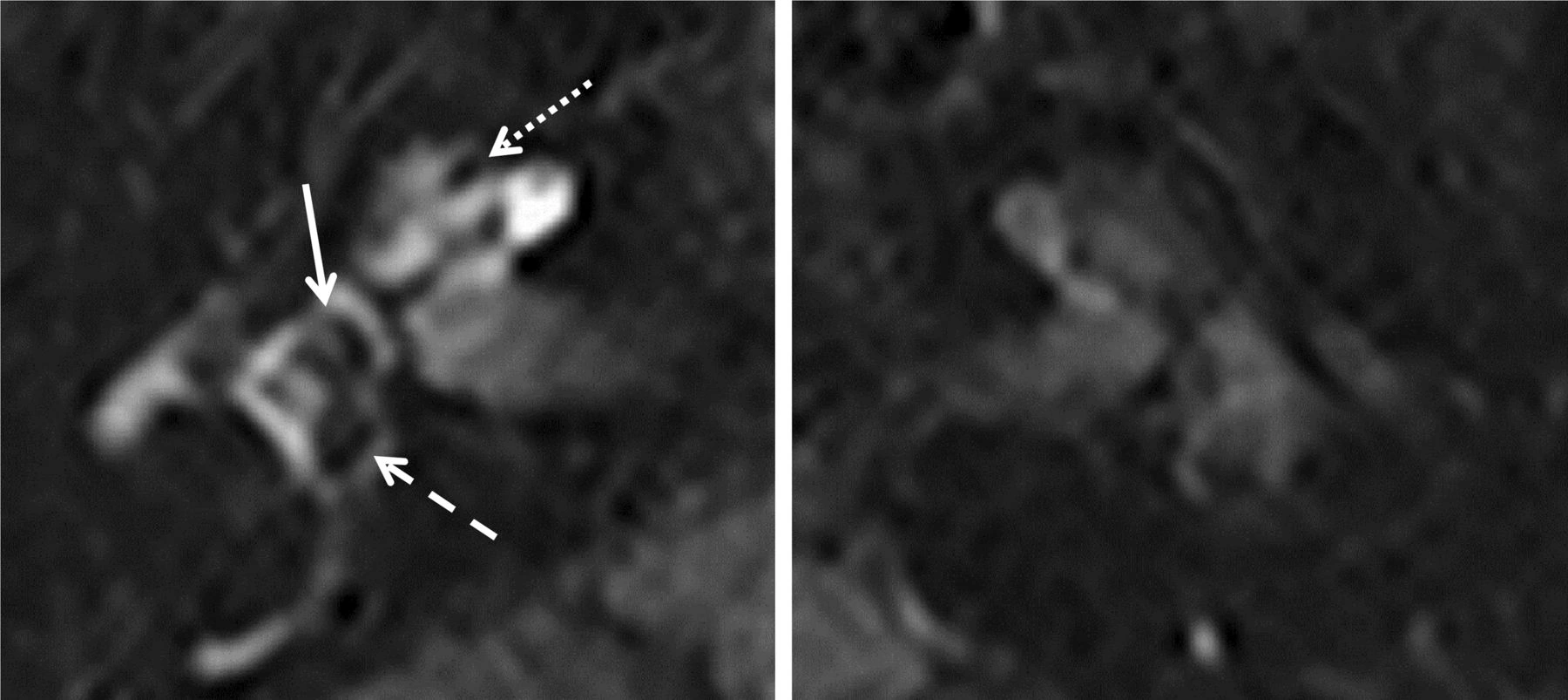
This is the workhorse of EH imaging. After an intravenous gadolinium injection, the scan is performed about four hours later. The contrast fills the perilymph, making it bright on the 3‑D FLAIR images while the endolymph stays dark—so the “hydrops” stands out like a shadow in a bright room.
According to a 2024 study in the Egyptian Journal of Radiology, the technique achieved a 97 % detection rate on a 1.5 T magnet—meaning you don’t always need a pricey 3 T scanner to get reliable results (rel=”nofollow noreferrer” target=”_blank”>https://ejrnm.springeropen.com/articles/10.1186/s43055-024-01309-9).
3D‑CISS Sequence
If you want crystal‑clear detail of the semicircular canals and vestibule, the CISS sequence is your go‑to. It’s especially helpful when the hydrops is subtle or when you need to rule out other structural anomalies. While it’s most commonly run on a 3 T scanner, many centers have adapted it for 1.5 T with acceptable quality.
SURI Grading
The Saccule‑Utricle Ratio Inversion (SURI) is a semi‑quantitative score that compares the size of the saccule to the utricle on axial 3‑D‑FLAIR images. A positive SURI (SURI+) strongly correlates with the symptomatic ear and higher hearing loss. In a 2023 Frontiers Neurology paper, SURI was the best predictor of disease side, outperforming other MRI criteria (rel=”nofollow noreferrer” target=”_blank”>https://www.frontiersin.org/articles/10.3389/fneur.2023.1105461/full).
Interpreting the Images
Vestibular vs. Cochlear Hydrops
In most patients, the vestibular system (the balance part) shows more pronounced hydrops than the cochlea (the hearing part). One consensus report found that the vestibule was more severely affected in nearly 60 % of cases. That’s why you’ll often see a “vestibular‑dominant” pattern on the scan, especially in classic Ménière’s disease.
Quantitative Grading
Beyond visual inspection, radiologists can calculate the EH %—the proportion of the endolymphatic space to the total inner‑ear volume. Higher percentages line up with worse vertigo and bigger pure‑tone averages. A 2023 Eur Arch Otorhinolaryngol study showed a direct link between EH % and disease duration, which helps clinicians gauge how far the process has progressed.
Pitfalls to Watch
Timing is everything. Scanning too early (say, 30 minutes after contrast) can miss subtle hydrops because the gadolinium hasn’t fully diffused into the perilymph yet. Motion artifacts—especially from patients who feel dizzy—can blur the delicate structures. Finally, false positives can happen if the contrast leaks into the endolymph (very rare, but worth a mention).
When to Order the Scan
Here’s a quick cheat‑sheet to help you decide if an Meniere disease diagnosis work‑up might benefit from an MRI:
| Clinical Scenario | Why MRI Helps |
|---|---|
| Classic Ménière’s symptoms (spells of vertigo, fluctuating hearing loss, tinnitus) | Confirms EH, guides targeted therapies like intratympanic steroids. |
| Unexplained fluctuating hearing loss without clear vertigo | Detects covert cochlear hydrops—may prevent unnecessary surgery. |
| Recurrent vertigo that doesn’t fit vestibular migraine | Distinguishes vestibular hydrops from migraine‑related dizziness (vestibular migraine diagnosis). |
| Pre‑operative planning for labyrinthectomy or vestibular neurectomy | Maps the extent of hydrops, improving surgical outcomes. |
Benefits vs. Risks – A Balanced View
Benefits
- Objective evidence: No more guessing—your doctor can see the hydrops.
- Tailored treatment: From medication to surgery, decisions become data‑driven.
- Monitoring tool: Repeat scans can track disease progression or treatment response.
Risks & Limitations
- Gadolinium safety: While generally safe, patients with severe kidney disease should be screened for nephrogenic systemic fibrosis (FDA guidance).
- Access & cost: Not every radiology center has the dedicated 3‑D sequences; insurance coverage varies.
- False‑negatives: About 5‑10 % of clinically diagnosed Ménière’s patients show no hydrops on MRI; the scan isn’t a 100 % rule‑out.
How to Prepare (Patient‑Focused)
Preparing for an Endolymphatic Hydrops MRI isn’t rocket science, but a few simple steps smooth the journey:
- Check kidney function: If you have a history of kidney disease, let your physician know; they may order a quick blood test.
- Fasting: Most centers ask you to skip food for 4‑6 hours before the contrast injection.
- Medication review: Certain drugs (e.g., metformin) might need a brief pause—ask your doctor.
- Stay still: The scan lasts ~20 minutes; a pillow or gentle music can help keep you relaxed.
After the injection, you’ll wait about four hours before the actual scan. It feels a bit like waiting for a latte to steep—except the payoff is a clear view of your inner ear.
Real‑World Example
Imagine Jane, a 48‑year‑old teacher who started experiencing “the room spinning” episodes three times a month, paired with sudden hearing drops in her right ear. Her ENT suspected Ménière’s disease but wanted proof before starting invasive therapy. Jane underwent an Endolymphatic Hydrops MRI on a 3 T scanner, and the images showed a pronounced SURI+ in her right vestibule, with an EH % of 55 %—a clear sign of vestibular hydrops. Based on those results, her doctor started a regimen of low‑salt diet, intratympanic steroids, and vestibular rehab. Within six weeks, Jane’s vertigo episodes halved, and her hearing stabilized.
Stories like Jane’s illustrate why the scan isn’t just a fancy picture—it can be the turning point for a treatment plan.
Future Directions
Science never sleeps, and the world of inner‑ear imaging is buzzing with innovation:
- Ultra‑high‑field 7 T MRI: Researchers are testing sub‑voxel resolution to map even tiny pockets of hydrops.
- Artificial‑Intelligence segmentation: Early AI models can automatically calculate EH % in seconds, reducing inter‑observer variability.
- Therapeutic trials: Some studies are using MRI grades to predict who will respond best to intratympanic steroids.
For those keeping an eye on the horizon, these advances promise even sharper diagnostics and more personalized care.
Conclusion
Endolymphatic Hydrops MRI has transformed how we look at dizzy‑related disorders. By converting an invisible fluid imbalance into a vivid, measurable image, it empowers doctors—and you—to make smarter, safer decisions. While the gadolinium contrast carries a tiny risk, the diagnostic payoff—earlier symptom control, clearer prognoses, and a roadmap for treatment—far outweighs it. Whether you’re navigating Ménière’s disease, a puzzling case of fluctuating hearing loss, or trying to rule out vestibular migraine, this scan can be the lighthouse that guides you out of the fog.
So, the next time your doctor mentions “Endolymphatic Hydrops MRI,” you’ll know exactly what to expect and why it matters. If you have any lingering questions, feel free to explore the related topics on vestibular hydrops MRI, cochlear hydrops MRI, or dive deeper into the vestibular migraine diagnosis. Remember, knowledge is the first step toward relief, and you’re not alone on this journey.























Leave a Reply
You must be logged in to post a comment.