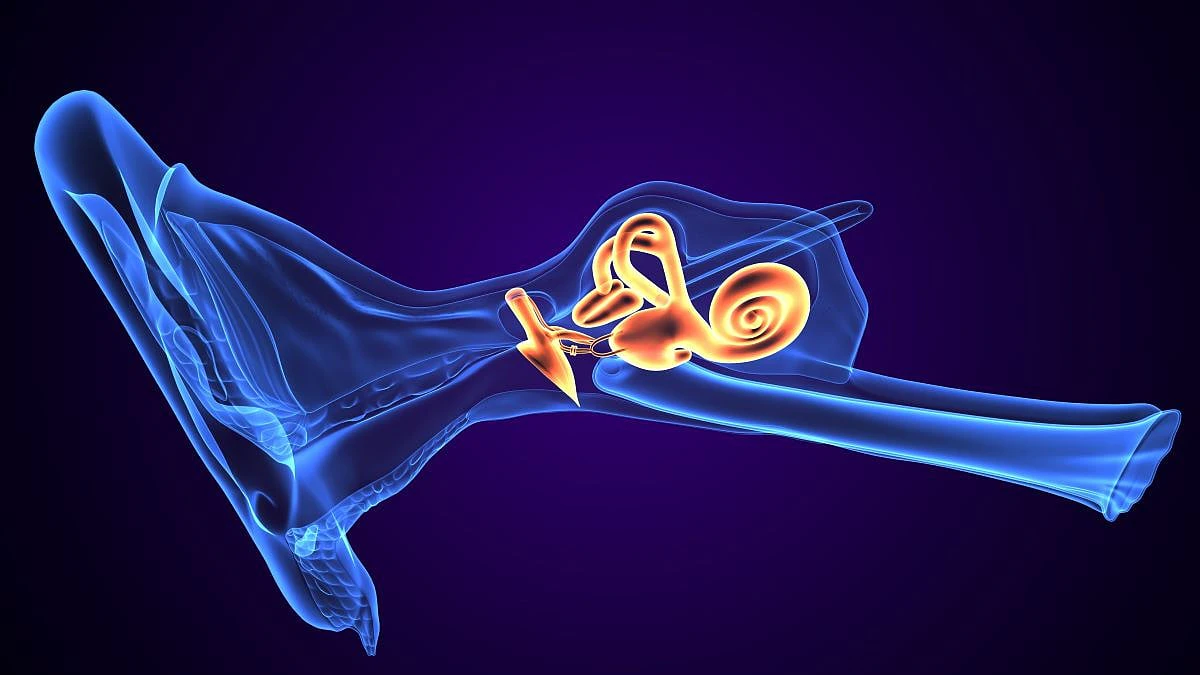
Hey there, fellow ear‑nerd! If you’ve ever felt that dizzy, spinning sensation that just won’t quit, or you’ve been told you might have “Meniere’s disease” or “vestibular migraine” and are left scratching your head, you’re in the right place. In the next few minutes we’ll unpack the magic of vestibular hydrops MRI – a scan that can actually see the fluid imbalance inside your inner ear. No jargon‑filled lecture, just a friendly chat that gets you the answers you need, fast.
Quick Answer
The vestibular hydrops MRI is a specialized, contrast‑enhanced magnetic resonance scan that visualises excess endolymph (the fluid inside the vestibular labyrinth). When that fluid balloons, the test lights it up as a dark pocket against bright perilymph, letting doctors tell whether you have true Meniere’s disease, vestibular migraine, or something else. In practice, it can confirm the diagnosis with about 80 % accuracy and guide the next step of treatment.
Clinical Importance
Why should you care about a scan that most of us have never heard of? Because the difference between “Meniere’s disease” and “vestibular migraine” isn’t just academic – it determines whether you’re headed for a diet change, a medication, or maybe even a surgical conversation.
Endolymphatic hydrops – the buildup of fluid in the inner ear – was first described in the lab by Hallpike in the 1950s. Decades later, researchers discovered that you could actually see this swelling on MRI. According to a 2020 narrative review, hydrops is present in 99.4 % of definite Meniere’s cases, but it also shows up in a surprising 12‑31 % of healthy ears, so we have to interpret it carefully.
When the scan shows both vestibular and cochlear hydrops (sometimes called VEH + CEH), the odds swing heavily toward classic Meniere’s disease. If the scan is clean, especially in someone with normal hearing, vestibular migraine becomes the more likely culprit. This helps avoid unnecessary earbuds of “maybe it’s Meniere’s, maybe it’s something else,” and gets you the right care faster.
Scan Procedure
Wondering what actually happens on the day of your scan? Here’s the low‑down, broken into bite‑size steps.
Preparation
You don’t need to fast, but you should let the tech know about any metal implants or a history of kidney issues (gadolinium, the contrast we use, is cleared by the kidneys). Most people feel perfectly fine – it’s just a short walk into the scanner.
Contrast administration
There are two ways to get the gadolinium into your inner ear:
- Intravenous (IV) injection: A standard dose (0.1 mmol/kg) is given, and the images are taken about 4 hours later. This is the most common method and works well on a 3 T scanner.
- Intratympanic (IT) injection: A tiny amount of contrast is placed through the eardrum, then scanned 24 hours later. It can be a little more sensitive, but it’s less widely available. Animal studies (Nonoyama 2016) have shown it isn’t ototoxic.
Scanning protocol
Most modern centres use a 3 Tesla (3 T) MRI because the higher magnetic field gives clearer detail – think of it as swapping a blurry TV for a 4K screen. The typical sequence is a 3‑D FLAIR or SPACE scan with voxel sizes around 0.6 mm. The whole acquisition lasts 5‑7 minutes, but there’s a little extra time for the technician to set things up.
Reading the images
Radiologists grade the amount of hydrops from 0 (none) to 3 (severe) for both the vestibular organ and the cochlea. A subtraction technique makes the perilymph glow white and the endolymph stay black, giving that striking “dark‑inside‑a‑bright‑cave” look that signals fluid overload.
Safety & side‑effects
Gadolinium reactions are rare, and the intratympanic route can cause a brief feeling of fullness in the ear – nothing lasting longer than a few hours. As always, let your doctor know if you’ve had any allergic reactions to contrast before.
Reading the Scan
Now that you know how the pictures are made, let’s talk interpretation – what does a “positive” or “negative” result really mean for you?
Positive vestibular hydrops (VEH +)
Seeing a dark pocket in the vestibular labyrinth is a strong clue for Meniere’s disease, especially when the cochlea is also involved. It usually translates to a treatment plan that may include salt restriction, diuretics, or targeted intratympanic gentamicin to quiet the troublesome spins.
Cochlear hydrops only (CEH +)
If the scan lights up just the cochlea, you might be dealing with an early stage of Meniere’s or a condition that mainly affects hearing. Lifestyle changes and hearing‑preserving meds become the focus. Read more about cochlear hydrops MRI for a deeper dive.
No hydrops detected
A clean scan doesn’t automatically rule out Meniere’s – about 20 % of histologically proven cases don’t show up on MRI. In that scenario, doctors will usually go back to the bedside: detailed vestibular testing, careful symptom tracking, and perhaps a trial of migraine prophylaxis. Vestibular migraine diagnosis guidelines can be helpful here.
Mixed findings (VEH + & CEH)
When both compartments are swollen, you’re looking at classic Meniere’s disease – the “full‑house” pattern. Evidence suggests these patients have a higher risk of progressive hearing loss, so early intervention is often recommended. Meniere disease diagnosis resources cover the next steps.
Benefits & Risks
| Aspect | Benefit | Risk / Limitation |
|---|---|---|
| Diagnostic clarity | Objective confirmation of hydrops; guides targeted therapy. | False‑positives in healthy ears (up to 31 %). |
| Treatment planning | Helps decide between medication, diet, or interventions. | Limited availability – many centres lack 3 T protocols. |
| Safety | IV gadolinium is non‑ototoxic; IT route safe in animal studies. | Rare allergic reactions; intratympanic injection can cause temporary fullness. |
| Cost | Potentially reduces expensive, unnecessary work‑ups. | Out‑of‑pocket $500‑$1500 in the US; insurance coverage varies. |
Balancing these pros and cons is a shared decision‑making process between you and your specialist. According to a 2022 study in Otology & Neurotology, using a standardized 3 T protocol can shave 40 % off artefact‑related errors, making the test more reliable.
Case Studies
Classic Meniere’s – mixed VEH + CEH
Maria, 48, had three years of vertigo attacks, low‑frequency hearing loss, and a feeling of fullness in her right ear. The MRI showed grade 3 vestibular hydrops and grade 2 cochlear hydrops. After a gentle intratympanic gentamicin regimen, her spells stopped within a month. She now lives a normal life and swears by her low‑salt diet.
Vestibular migraine mimic
James, 32, experienced episodic vertigo with perfectly normal hearing. His scan was clean – no hydrops at all. The physician pivoted to a vestibular migraine work‑up, started venlafaxine, and James reported a 70 % reduction in attacks after six weeks.
Negative MRI but histologic hydrops
Linda, 61, met the AAO‑HNS criteria for definite Meniere’s, yet her 3 T scan showed no hydrops. The doctor explained the false‑negative rate and prescribed a trial of diuretics, which helped control her symptoms. This case underscores that clinical judgment still matters.
Unilateral disease, bilateral MRI signs
Mark, 55, complained of vertigo only on his left side. The MRI, however, revealed vestibular hydrops in both ears – the so‑called “vestibular aqueduct sign.” He learned that subclinical disease can be present in the opposite ear and now monitors both ears with regular audiograms.
Technical pitfall – artefact mistaken for hydrops
During a routine scan, a patient’s motion caused a bright artefact that looked like perilymph. The radiologist caught the mistake, repeated the scan, and the second study was clean. The lesson? Always double‑check image quality before finalising the report.
Future Research
Science never sleeps. Researchers are now exploring Radiomics – a fancy AI technique that analyses texture patterns in MRI beyond the human eye. Early data suggest it could boost diagnostic accuracy to over 90 %. Another hot topic is low‑dose intratympanic gadolinium, which may make the scan even safer for repeated use.
There’s also a push for a universal reporting checklist, sometimes called the “Hydrops MRI Score,” to standardise how we describe findings across hospitals. If you’re curious about the technical side, you can read more about Endolymphatic hydrops MRI on our site.
Quick Checklist
| Step | What to Do |
|---|---|
| 1️⃣ Clinical suspicion | Complete AAO‑HNS criteria for Meniere’s or vestibular migraine. |
| 2️⃣ Talk to your doctor | Ask if a vestibular hydrops MRI is available at a 3 T centre. |
| 3️⃣ Safety screen | Check kidney function and any gadolinium allergies. |
| 4️⃣ Choose contrast route | IV is standard; IT may be considered for research settings. |
| 5️⃣ Get the scan | Follow prep instructions; relax during the 5‑minute acquisition. |
| 6️⃣ Interpret results | Use the grading scale (0‑3) for vestibular and cochlear hydrops. |
| 7️⃣ Plan treatment | Match therapy to the pattern (diet, meds, injections, rehab). |
| 8️⃣ Follow‑up | Re‑scan if symptoms evolve after 12 months. |
Final Thoughts
Living with fluctuating vertigo or hearing loss can feel like being stuck on a roller coaster you never signed up for. The good news? Vestibular hydrops MRI gives us a window into the inner ear that was once only accessible in a lab after death. By turning that invisible fluid overflow into a clear picture, the scan helps you and your doctor make smarter, faster decisions – whether that means lifestyle tweaks, medication, or in rare cases, surgery.
Remember, the scan isn’t a magic wand, but it’s a powerful tool in a toolbox that also includes thorough history taking, bedside tests, and sometimes a bit of trial‑and‑error. If you think you might benefit, have a candid conversation with your otolaryngologist. Ask about the availability of a 3 T vestibular hydrops MRI, the contrast options, and what the findings could mean for your next steps.
Got questions? Have you already gone through a hydrops MRI and want to share your experience? I’d love to hear from you – feel free to reach out. Here’s to clearer scans, calmer ears, and a steadier world.























Leave a Reply
You must be logged in to post a comment.