How is vestibular migraine diagnosed? In short, doctors combine a detailed story about your symptoms with a set of internationally‑approved criteria. There’s no single blood test or scan that says “yes, this is VM”, but when the pieces fit together you get a solid diagnosis that can finally guide treatment.
Getting the right label matters. It spares you from endless ear‑doctor visits, unnecessary scans, and the frustration of being told “it’s all in your head”. Instead, a proper vestibular migraine diagnosis opens the door to targeted meds, lifestyle tweaks, and—most importantly—relief.
What is vestibular migraine
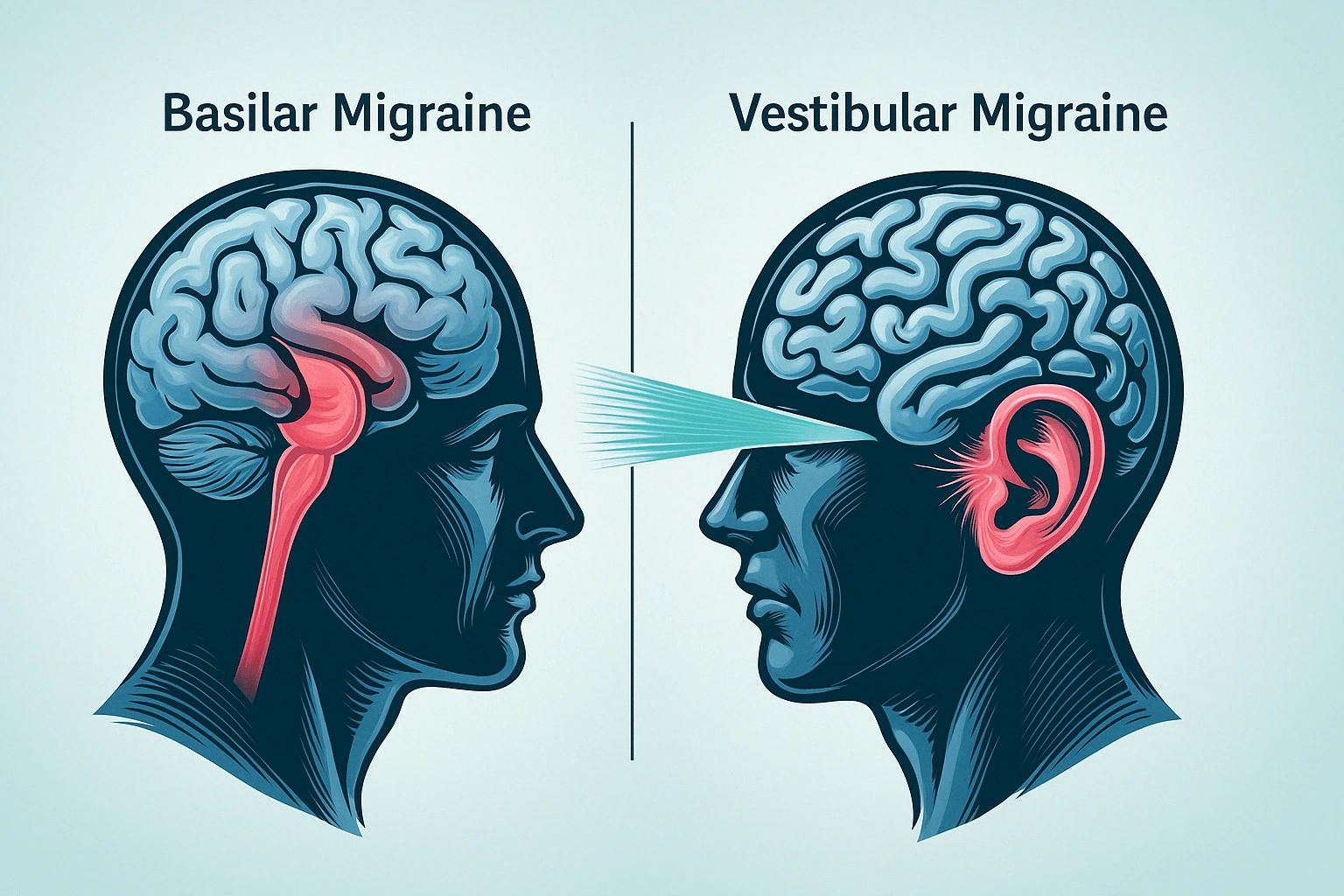
Think of vestibular migraine (VM) as the love‑child of two familiar foes: classic migraine and the inner‑ear balance system. Neurologically, migraine isn’t just a pounding headache; it can also tumble the vestibular apparatus that helps us stay upright. When the two collide, you get vertigo, dizziness, and a whole host of sensory quirks.
VM is surprisingly common. Roughly 40 % of people who experience migraine will also feel some vestibular disturbance at some point, and about 1 % of the general population meets the full diagnostic criteria for VM (Migraine Canada, 2024). It often shows up in women between 30 and 50, but anyone can be affected.
Why does it slip through the cracks? Because vertigo is also a hallmark of many ear‑related disorders—Meniere’s disease, vestibular neuritis, even benign paroxysmal positional vertigo (BPPV). Without a clear roadmap, patients and providers can end up chasing the wrong diagnosis for months.
Official diagnostic criteria
The gold‑standard comes from the International Headache Society and the Bárány Society. Their 2022 consensus (see the study in Journal of Vestibular Research) spells out exactly what clinicians need to see.
Definite vs. probable VM
There are two buckets:
- Definite vestibular migraine – all criteria are met.
- Probable vestibular migraine – most criteria are met, but one piece is missing (often the migraine feature during at least half of the attacks).
Step‑by‑step checklist
| Criterion | Definite VM | Probable VM |
|---|---|---|
| ≥ 5 vestibular episodes | ✔︎ | ✔︎ |
| Episode length 5 min – 72 h | ✔︎ | ✔︎ |
| History of migraine (ICHD) | ✔︎ | ✔︎ |
| ≥ 50 % of episodes with migraine feature (headache, photophobia, phonophobia, aura) | ✔︎ | – |
| No better explanation (e.g., Meniere, central lesion) | ✔︎ | ✔︎ |
Notice the emphasis on “vestibular symptoms of moderate or severe intensity”. Lightheadedness or a faint feeling alone isn’t enough; you need true vertigo, imbalance, or visually‑induced motion sickness.
How doctors apply the criteria
During the first visit, the clinician will ask you to describe:
- What the dizziness feels like (spinning vs. feeling off‑balance).
- How long each spell lasts.
- Any headache or migraine aura that shows up before, during, or after the vertigo.
- Triggering factors—bright lights, certain foods, stress, hormonal changes.
Between attacks, many patients have a completely normal neurological exam. That’s why the story you tell is the true diagnostic engine.
Key differential diagnosis
Before sealing the VM label, doctors must rule out a few look‑alikes. Below is a quick comparison that can help you understand what they’ll be checking.
| Feature | Vestibular migraine | Meniere disease diagnosis | Hydrops on MRI (endolymphatic/vestibular) |
|---|---|---|---|
| Hearing loss | Rare, usually none | Fluctuating, low‑frequency | Visible endolymphatic fluid accumulation |
| Tinnitus | Occasional, mild | Common, often pulsatile | May be present |
| Attack duration | 5 min – 72 h | Hours to days, often > 24 h | Variable, depends on fluid build‑up |
| Typical triggers | Light, stress, certain foods | Salt, barometric pressure | Progressive fluid shifts |
If you’ve ever been told you might have “Meniere disease”, you can read a more detailed comparison here: Meniere disease diagnosis. The key is the presence of hearing changes—if your ears stay quiet, VM becomes more likely.
When imaging is called for, clinicians may order an Endolymphatic hydrops MRI or a Vestibular hydrops MRI to visualize fluid in the inner ear. A Cochlear hydrops MRI is useful when hearing loss is the main complaint.
When to image
Remember: imaging is not a requirement for classic VM. It’s reserved for “red‑flag” situations.
Red‑flag signs that demand a scan
- Sudden, severe neurological deficits (weakness, numbness, speech trouble).
- Persistent unilateral hearing loss.
- Symptoms that don’t fit the VM timeline—e.g., episodes lasting weeks.
- A history of stroke, tumor, or other central nervous system disease.
If any of those pop up, a brain MRI (often with contrast) is ordered to rule out structural causes.
Typical imaging pathway
- Brain MRI – rule out demyelination, tumors, vascular lesions.
- Inner‑ear MRI (high‑resolution 3 T) – looks for endolymphatic or vestibular hydrops.
- Targeted ear‑specific MRI – if hearing loss is present, focus on cochlear structures.
When the MRI comes back clean and your story matches the criteria, the vestibular migraine diagnosis is confirmed.
Practical clinical workflow
Below is a typical patient journey, broken down into bite‑size steps. Feel free to print this out or save it in a notes app.
| Visit | What the doctor does | What you bring |
|---|---|---|
| Initial consult | Comprehensive history, symptom diary review, migraine questionnaire. | Headache diary, list of triggers, current meds. |
| Physical exam | Bedside vestibular tests (Dix‑Hallpike, head‑impulse). | Comfortable shoes, willingness to stand. |
| Follow‑up (2‑4 weeks) | Review diary, apply ICHD criteria, assess red‑flags. | Updated diary, note any new symptoms. |
| Imaging (if needed) | Order brain MRI or inner‑ear MRI. | Previous imaging reports, insurance info. |
| Diagnosis discussion | Explain “definite” or “probable” VM, outline treatment plan. | Questions, consent for meds or rehab. |
Real‑world example
Emily, a 38‑year‑old graphic designer, visited her neurologist after three months of “spinning episodes” that lasted about an hour each. She also reported occasional throbbing headaches with light sensitivity. Her ear exam was normal, and an MRI showed no lesions. By applying the criteria table above, the doctor identified a definite VM diagnosis. Emily started a low‑dose beta‑blocker and a vestibular rehab program and saw a 70 % reduction in episodes within three months.
After the diagnosis
Now that you have a label, treatment moves into the spotlight. The goal is two‑fold: stop the attacks and lower their frequency.
Acute remedies
- Triptans (e.g., rizatriptan) – work well if taken early.
- NSAIDs – ibuprofen or naproxen can dull the pain and nausea.
- Anti‑emetics – meclizine or ondansetron for severe vertigo.
Preventive options
Preventive meds are chosen based on your overall migraine profile, comorbidities, and side‑effect tolerance. Common choices include:
- Beta‑blockers (propranolol).
- Calcium channel blockers (verapamil).
- CGRP monoclonal antibodies – a newer class that’s shown promise for VM in recent NeurologyLive studies.
Lifestyle tweaks that actually help
It sounds cliché, but sleep, hydration, and stress management are the backbone of migraine control.
- Regular schedule – aim for the same wake‑up and bedtime.
- Limit triggers – common culprits: caffeine, aged cheese, alcohol, and bright flashing lights.
- Vestibular rehab – graded balance exercises prescribed by a physical therapist can reduce dizziness over weeks.
- Dietary notes – some patients feel better with a low‑sodium diet (helps differentiate from Meniere’s) and magnesium‑rich foods.
Questions you might ask your doctor
- What defines “definite” versus “probable” in my case?
- Do I need any imaging, or is my story enough?
- Which preventive medication aligns with my health history?
- Can I start vestibular rehab while on meds?
- How will we track progress?
Having these questions ready shows you’re an active partner in your care—a factor that research shows improves outcomes.
Wrapping it up
Diagnosing vestibular migraine is a bit like solving a puzzle. You gather the pieces—vertigo episodes, migraine clues, and a careful exclusion of ear disorders—then fit them together using the internationally‑validated criteria. When the picture is complete, you finally have a name for the condition that’s been stealing your balance and peace of mind.
Remember, the journey doesn’t end with the label. With the right treatment plan, lifestyle adjustments, and maybe a little vestibular rehab, most people see a dramatic drop in attack frequency and intensity. If you suspect you’re dealing with VM, reach out to a neurologist or an ENT who is familiar with the Bárány/IHS criteria. Bring a symptom diary, ask the questions above, and let the conversation guide you toward relief.
What’s your experience with dizzy spells? Have you found a treatment that works wonders, or are you still searching for answers? Share your thoughts with a trusted friend or a support community—sometimes just talking it out is the first step toward feeling steady again.






















Leave a Reply
You must be logged in to post a comment.