Headaches come in many forms, such as tension headaches, migraines, ice pick headaches, and others. The trigger, length, and severity differ depending on the type.
Most people have experienced that pulsing, unpleasant, and distracting head pain at some point. There are several distinct headache varieties. The common ones include:
- tension headache
- cluster headache
- migraine headache
- hemicrania continua
- ice pick headache
- thunderclap headache
- allergy or sinus headache
- hormone headache (also called menstrual migraine)
- caffeine headache
- exertion headache
- hypertension headache
- rebound headache
- post-traumatic headache
- spinal headache
Seek urgent medical careSometimes a headache demands immediate medical evaluation. Get urgent care if you have any of the following symptoms along with your headache:
- stiff neck
- skin rash
- the worst headache you’ve ever experienced
- vomiting
- confusion
- slurred speech
- fever of 100.4°F (38°C) or higher
- paralysis of any body part
- loss of vision
If your headache is milder, continue reading to learn how to identify the likely type and what steps you can take to relieve symptoms.
What are the most common types of primary headaches?
Primary headaches are those where the head pain itself is the main disorder, not a result of another medical issue such as an infection or allergy.
These headaches may be episodic or chronic:
- Episodic headaches occur intermittently and not more than in a single month. They can last from about half an hour to several hours.
- Chronic headaches are more persistent, happening more than 15 days per month. These cases generally require a pain management strategy.
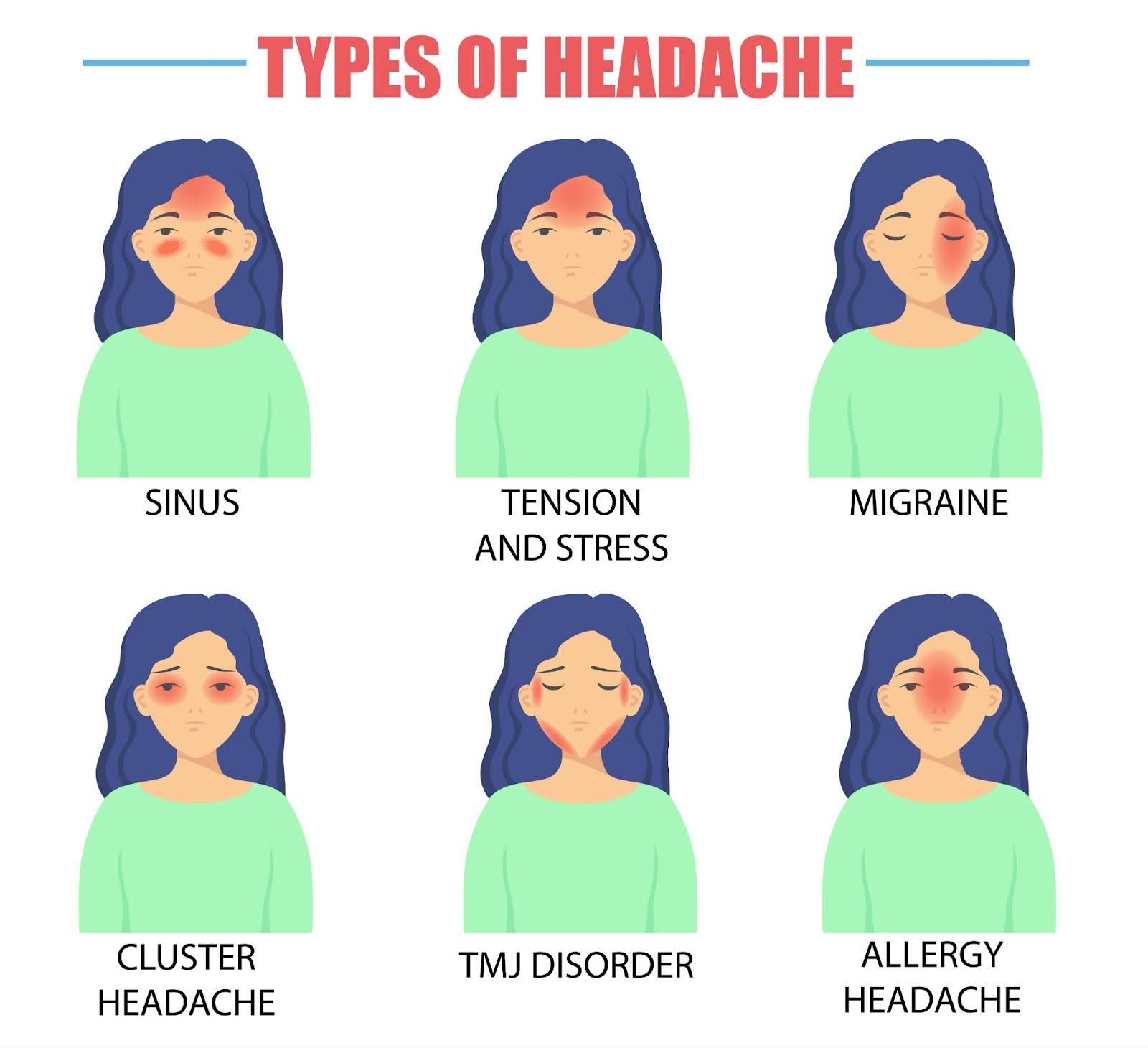
The diagram above is a general guide to where headaches can appear, though many may occur outside the highlighted zones.
Tension headache
Tension headaches typically cause a dull, aching discomfort across the head. You may also notice tenderness or sensitivity around the neck, forehead, scalp, or shoulder muscles.
Anyone can develop tension headaches. They are commonly triggered by stress.
Cluster headache
Cluster headaches bring intense, burning, and piercing pain. They typically affect the area around or behind a single eye or one side of the face at a time. Associated symptoms can include:
- swelling, redness, flushing, or sweating on the side affected by the headache
- nasal congestion and tearing of the eye on the same side as the pain
These headaches come in bouts. Each episode can last from . During a cluster period, people may have headaches anywhere from per day, often at similar times each day. One headache subsides and another quickly replaces it.
Clusters can persist daily for months. Between bouts, people are symptom-free. Cluster headaches are in spring and fall and tend to be more common in men.
Clinicians do not fully understand why cluster headaches occur.
Migraine
Migraine is a headache disorder marked by intense, throbbing pain deep in the head. Untreated attacks can last between 4 and 72 hours and significantly hinder daily functioning. During an attack, you may have:
- pulsing pain, often focused on one side of the head
- sensitivity to light
- sensitivity to sound
- nausea and vomiting
About of people with migraine experience visual changes prior to the headache phase. This migraine aura can make you see:
- flashing or shimmering lights
- zigzag patterns
- stars
- blind spots
Auras can also include numbness or tingling on one side of the face or in one arm and difficulty speaking.
Possible emergencyStroke symptoms may resemble a migraine. If you notice new neurological symptoms, seek immediate medical help.
Migraine often runs in families and can be linked to other nervous system disorders. According to the National Institute for Neurological Disorders and Stroke (NINDS), people assigned female at birth are to develop migraine compared with those assigned male at birth. Individuals with post-traumatic stress disorder (PTSD) also have an of developing migraine.
Common migraine triggers include environmental and lifestyle factors such as:
- sleep disturbances
- dehydration
- skipping meals
- certain foods
- hormonal shifts
- exposure to chemicals
Hemicrania continua
Hemicrania continua is a steady, moderate headache affecting one side of the head that persists continuously for at least . You may notice episodes of increased pain several times daily.
Researchers believe it accounts for about of headaches and is most common in younger adults.
This headache type can also be accompanied by:
- tearing or red eyes
- nasal congestion or runny nose
- drooping eyelid
- forehead sweating
- miosis, or excessive pupil constriction
- restlessness or agitation
Ice pick headache
Primary stabbing headaches, commonly called ice pick headaches, are brief, intense stabbing pains in the head that last only a few seconds.
They can occur several times a day and strike without warning. An ice pick headache may feel like a single stab or multiple stabbing sensations in quick succession.
These headaches often move around to different areas of the head. If your ice pick headaches consistently appear in the same spot, it could indicate an underlying condition.
Thunderclap headache
A thunderclap headache is an extremely severe head pain that reaches peak intensity in less than a minute. While it can be harmless, it may also signal a serious medical issue requiring prompt attention.
Possible causes include:
- blood vessel tears, ruptures, or blockages
- stroke
- brain trauma
- reversible cerebral vasoconstriction syndrome (RCVS)
- vasculitis (blood vessel inflammation)
- pituitary apoplexy (bleeding into or sudden loss of blood from the pituitary)
If you experience a thunderclap headache for the first time, seek urgent medical care. If another condition is ruled out, your doctor can discuss treatment options for future episodes.
What are the most common types of secondary headaches?
Secondary headaches are symptoms of another issue in your body. If the trigger persists, these headaches can become chronic. Treating the underlying cause typically relieves the headaches.
Allergy or sinus headache
Headaches sometimes arise from allergic reactions. Pain is commonly centered around the sinuses and front of the head.
Migraine is frequently mistaken for sinus headaches. Individuals with chronic seasonal allergies or sinusitis are more prone to these headaches.
Hormone headache
People who menstruate may experience headaches related to hormonal changes. Menstruation, oral contraceptive use, and pregnancy all alter estrogen levels and can precipitate headaches.
Headaches tied to the menstrual cycle are often called menstrual migraines. They typically occur between your period and the third day of bleeding, and sometimes around ovulation.
Caffeine headache
Caffeine influences cerebral blood flow. Too much intake can trigger a headache, as can abrupt cessation. People who frequently have migraines are at risk for caffeine-related headaches.
If your brain is accustomed to a certain daily amount of caffeine, you may develop a headache when that intake stops. This may be due to changes in brain chemistry brought on by the stimulant, making withdrawal a trigger.
Exertion headache
Exertion headaches occur soon after intense physical exertion. Activities such as heavy lifting, running, and sexual activity often trigger them. These activities likely increase blood flow to the head, producing a throbbing pain on both sides.
An exertion headache usually resolves fairly quickly — within a or a few hours.
They can sometimes be due to a secondary cause. If exertion headaches are new or last longer than expected, seek medical evaluation.
Hypertension headache
Severely elevated blood pressure can cause headache and is considered an emergency. This type of headache may appear when blood pressure reaches dangerous levels (greater than 180/120). In most people, high blood pressure does not produce headaches.
A hypertension headache usually affects both sides of the head and worsens with activity. It often has a pulsating character.
Medical emergencyIf you suspect a hypertension headache, get emergency care. Call 911 or go to the nearest ER if you have:
- vision changes
- numbness or tingling
- nosebleeds
- chest pain
- shortness of breath
You’re more likely to get this headache if you are already being treated for high blood pressure.
Medication overuse headache
Medication overuse headaches, or rebound headaches, may feel like a dull tension headache or a more severe migraine-type pain.
These are more likely in people who frequently use over-the-counter (OTC) pain relievers. Excessive use of these drugs leads to more headaches rather than fewer.
These headaches commonly occur when OTC medications are taken more than 15 days per month. Such OTC drugs include:
- acetaminophen
- ibuprofen
- aspirin
- naproxen
They’re also more common with medicines that contain caffeine.
Post-traumatic headache
Post-traumatic headaches can develop after any head injury and often resemble tension headaches or migraines. They typically last up to after the injury, but they can become chronic.
Spinal headache
Spinal headaches result from low cerebrospinal fluid pressure after a lumbar puncture, so they’re also called post-dural puncture headaches. You may feel the pain in your:
- forehead
- temples
- upper neck
- back of the head
Research suggests spinal headaches follow a lumbar puncture between of the time. They usually start within 2 to 3 days but can begin months later. They can also occur after an epidural or spontaneously.
This headache typically worsens when you stand and improves when you lie down.
Other symptoms of a spinal headache include:
- nausea
- neck pain
- dizziness
- vision changes
- tinnitus or ringing in the ears
- hearing loss
- radiating pain into the arms
When should I get help?
Most episodic headaches resolve within 48 hours. If a headache persists more than 2 days or becomes increasingly severe, consider consulting a physician.
If you experience headaches on more than 15 days per month for over 3 months, you may have a chronic headache disorder. Even if OTC treatments help, see a doctor for a diagnosis and management plan.
Headaches can indicate more serious health issues, and some need treatment beyond home remedies and OTC drugs.
If you need assistance locating a primary care physician, try our FindCare tool here.
How can I identify my headache?
A headache diagnosis usually starts with a physical exam and medical history. If possible, keep a “headache diary” in the weeks before your appointment. Record each headache’s:
- duration
- intensity
- location
- possible triggers
Because headaches vary widely, multiple approaches may be needed to determine the type you have. Doctors need to know whether your headache is primary or secondary to recommend the right treatment.
Your primary care doctor may refer you to a specialist, such as a neurologist. Diagnostic tests sometimes required to find an underlying cause include:
- MRI or CT scan
- lumbar puncture
- blood tests
How do you manage and treat headaches?
Treatment varies by headache type and can range from dietary and lifestyle adjustments to medical procedures.
Not everyone responds the same way to treatments, even for the same headache type. If you cannot control your headaches alone, consult a doctor to develop a treatment plan.
Below are common treatments used for the various headache types.
Tension headache
OTC pain relievers often ease occasional tension headaches. These include:
- aspirin (Bayer)
- ibuprofen (Advil)
- naproxen (Aleve)
- acetaminophen and caffeine combinations
If OTC medicines are ineffective, a physician may prescribe drugs like:
- indomethacin
- meloxicam (Mobic)
- ketorolac
For chronic tension headaches, a doctor may recommend treating underlying triggers.
Cluster headache
Doctors may suggest therapies or medications for symptom relief, including:
- oxygen therapy
- sumatriptan (Imitrex)
- local anesthetic (lidocaine)
After diagnosis, clinicians work on preventive strategies. Options that may induce remission of cluster periods include:
- corticosteroids
- melatonin
- topiramate (Topamax)
- calcium channel blockers
Migraine
If OTC drugs don’t relieve migraine pain during attacks, physicians may prescribe triptans, which reduce inflammation and alter cerebral blood flow. They’re available as nasal sprays, tablets, and injections.
Common triptans include:
- sumatriptan (Imitrex)
- rizatriptan (Maxalt, Axert)
Talk with your doctor about daily preventive medication if your headaches are:
- debilitating more than 3 days a month
- somewhat disabling 4 days a month
- lasting more than 6 days a month
A 2019 review found that preventive migraine drugs are underused: only 3 to 13% of people with migraine take preventive medication, while up to 38% might benefit from it.
Preventive treatment can greatly enhance quality of life and productivity.
Useful preventive medications include:
- propranolol (Inderal)
- metoprolol (Toprol)
- topiramate (Topamax)
- amitriptyline
- CGRP antagonists
Hemicrania continua
Hemicrania continua is notable for its complete responsiveness to indomethacin, an NSAID. A low dose taken with food typically eases symptoms within 24 hours.
Because indomethacin can cause side effects, especially at higher doses, doctors recommend the smallest effective amount.
Ice pick headache
Ice pick headaches are hard to treat because they’re so brief. Most resolve before much can be done.
Preventive treatments may reduce future frequency or severity. Options include:
- indomethacin
- gabapentin
- other NSAIDs, including COX-2 inhibitors
- melatonin
Thunderclap headache
If a thunderclap headache is caused by another condition, that condition must be treated.
If it’s a primary thunderclap headache, treatment options can include:
- NSAIDs like indomethacin
- calcium channel blockers
- beta-blockers
- topiramate
- lithium
- triptans
Allergy or sinus headache
Treatment focuses on thinning mucus and relieving sinus pressure. Options include:
- nasal steroid sprays
- OTC decongestants like phenylephrine (Sudafed PE)
- antihistamines such as cetirizine (Zyrtec)
A sinus headache may also indicate a sinus infection, in which case a doctor might prescribe medications to clear the infection and relieve symptoms. For more on causes that mimic migraine, see resources on left side head pain.
Hormone headache
OTC pain relievers like naproxen (Aleve) or prescription drugs such as frovatriptan (Frova) can help control pain.
Nonpharmacologic approaches in reducing monthly headache frequency. These may include:
- stress-reduction techniques and relaxation
- regular physical activity, like yoga
- good sleep habits
- modifying diet
- hormonal therapies, such as oral contraceptives
Caffeine headache
Maintaining a steady, moderate caffeine intake — or quitting gradually — can help prevent these headaches.
Exertion headache
OTC pain relievers like aspirin or ibuprofen (Advil) usually relieve symptoms.
If you frequently get exertion headaches, consult a doctor, as they can sometimes signal a more serious condition.
Hypertension headache
These headaches often improve with better blood pressure control and generally do not recur if hypertension is well managed.
Medication overuse headache
The treatment is to stop the overused medication. Although pain may worsen initially, it should resolve completely within a few days.
Using a daily preventive medication that doesn’t cause medication overuse headaches can help prevent recurrence.
Post-traumatic headache
Physicians commonly prescribe medications such as:
- triptans
- sumatriptan (Imitrex)
- beta-blockers
- amitriptyline
Spinal headache
Initial care usually includes pain relievers and hydration, and avoiding upright posture. Symptoms typically resolve on their own within one to two weeks.
In some cases, an epidural blood patch is used. A small amount of your blood is injected into the epidural space to help seal cerebrospinal fluid leaks and stop the headaches.
Can you prevent headaches?
Many headaches can be reduced or prevented by specific strategies, though prevention methods vary by headache type. Some medications may prevent one kind of headache while triggering another.
Discuss preventive options with your doctor to find the right plan. Prevention can decrease headache frequency, lessen severity, or stop headaches entirely.
Lifestyle changes that might prevent or improve headaches include:
- maintaining consistent, adequate sleep
- eating regularly and balanced meals
- staying well-hydrated
- regular physical activity
- managing stress
Migraine prevention may involve calcitonin gene-related peptide (CGRP) therapies. The FDA has approved a CGRP therapy, galcanezumab (Emgality), to prevent cluster headaches.
What’s the outlook for headaches?
Prognosis varies by headache type.
Primary headaches rarely cause permanent disability or death, though they can be severely disabling when frequent and intense. Most can be managed effectively once properly diagnosed and treated.
The outlook for secondary headaches depends on the underlying cause. Some improve with simple changes, while others can be life-threatening without prompt medical care.
If you have recurring or severe headaches, obtaining an accurate diagnosis is the essential first step toward understanding and managing them.
























Leave a Reply
You must be logged in to post a comment.