Wondering how steady your new lens will stay after cataract surgery? In most cases the intra‑ocular lens (IOL) stays locked in place, but even a few degrees of rotation can blur vision or reduce the astigmatic correction you were hoping for.
Below you’ll discover the factors that influence IOL stability, what the latest research says, and simple steps you and your surgeon can take to keep the lens exactly where it belongs. Let’s dive in together.
Why Stability Matters
How rotation changes visual outcomes
Imagine you’ve just got a brand‑new pair of glasses that are perfectly aligned – then they twist a little. That small twist can make everything look fuzzy. The same happens inside the eye. A study shows that a 5° rotation of a toric IOL can lose up to 30 % of its astigmatic correction, and a 10° turn can wipe out more than half of the intended effect. According to a systematic review, keeping rotation under 5° is the sweet spot for optimal vision.
Risks of an unstable IOL
When a lens isn’t stable you might notice glare, halos around lights, reduced sharpness, or even double vision. In extreme cases, the IOL can shift enough to require a second surgery. These problems are why surgeons and patients alike pay close attention to stability from day one.
Patient‑level factors
Age, the health of your capsular bag, previous eye trauma, or conditions like pseudo‑exfoliation can all affect how well the lens stays put. Knowing your own risk factors helps your surgeon choose the right equipment and plan.
Physics Behind Stability
Capsular bag – the natural home
The capsular bag is a thin, elastic membrane that once held your natural lens. After cataract removal, the IOL is tucked inside this bag, which acts like a snug pocket. If the bag is healthy and the lens fits well, the IOL tends to stay stable for years.
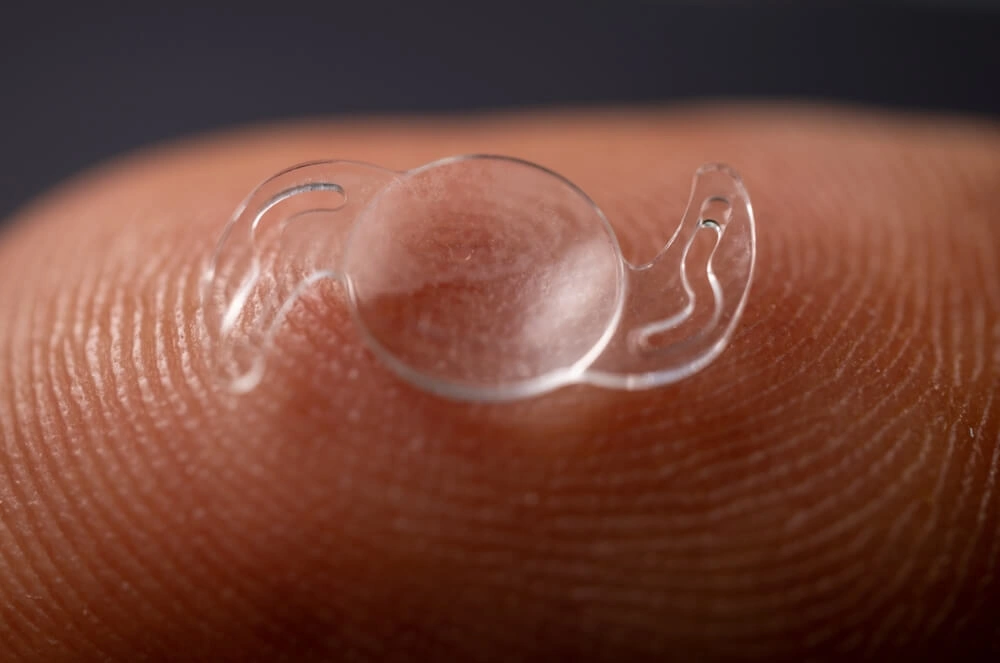
Haptic design and rotation control
Haptics are the tiny “arms” of the IOL that press against the capsular bag. Different designs—plate, C‑loop, frosted, or a mix—behave differently.
| Haptic Type | Typical Rotation | Pros | Cons |
|---|---|---|---|
| Plate (flat) | ≤ 3° | Excellent centration | May need larger capsular opening |
| C‑loop | 4‑6° | Easy to insert | Potential for slight wobble |
| Frosted | ≤ 2° (studies show) | High friction → less rotation | Manufacturing complexity |
| Plate + CTR | ≤ 2° | Best for weak zonules | Requires additional device |
Capsular tension ring (CTR) – the unsung hero
A capsular tension ring is a thin, flexible ring that sits inside the capsular bag, evenly distributing forces. When the bag’s zonules are weak—common in high‑myopia or after trauma—the CTR keeps the bag circular and reduces both tilt and rotation.
Light‑adjustable lenses – long‑term stability?
Light‑adjustable intraocular lenses (LALs) let surgeons fine‑tune the prescription post‑op using UV light. A 4‑year follow‑up of 43 eyes showed virtually no drift in position, proving that even after adjustments the lens can stay put for the long haul. Voptica’s report confirms this stability.
Evidence Based Review
Systematic review of toric IOL rotation
The big picture comes from a systematic review that pooled data from dozens of studies. It concluded that lens model and haptic design explain most of the variability in rotation, with frosted‑haptic and plate designs consistently outperforming standard C‑loop lenses.
Post‑market study of frosted‑haptic toric IOL
A 2022 clinical trial of a new toric IOL with frosted haptics reported an average rotation of just 1.6°, far below the 5° threshold. The authors noted that the textured surface creates a gentle “grip” on the capsular bag, limiting movement.
Vertical vs. horizontal ICL implantation
One large comparative study of toric implantable collamer lenses (ICL) found that vertical implantation resulted in a mean rotation of 1.11° compared with 3.02° for the traditional horizontal approach (p = 0.001). The researchers suggest that the vertical orientation aligns better with the natural anatomy of the sulcus, giving the lens extra stability. The PLOS ONE paper backs this up.
Extended‑Depth‑of‑Focus (EDOF) toric lenses
EDOF lenses add depth to near vision while correcting distance. A 2020 slit‑lamp image analysis showed mean rotation under 2°, comparable to standard toric lenses, meaning you don’t have to sacrifice stability for enhanced depth of focus.
Real‑world CTR implantation data
Clinicians who routinely add a CTR report a 30 % reduction in post‑operative rotation in eyes with zonular weakness. This practical evidence aligns with the biomechanical theory behind the ring’s stabilising effect.
Practical Surgeon Guide
Pre‑operative assessment
- Measure capsular bag size using ultrasound biomicroscopy; a larger bag may benefit from a CTR.
- Identify zonular laxity (e.g., pseudo‑exfoliation) – this flags a need for extra stabilisation.
- Choose the appropriate haptic design based on the patient’s anatomy and lifestyle.
Surgical technique tips
- Always aim for “in‑the‑bag” placement; sulcus positioning should be a backup, not the first choice.
- Perform gentle hydrodissection to keep the capsule intact and avoid tears that could let the lens wobble.
- Use a cohesive visco‑elastic that protects the bag but clears easily – residual visco can act like a lubricant, encouraging rotation.
Choosing the right IOL model
For patients with regular capsular bags, a plate‑haptic toric lens often gives the best rotation control. If you have mild zonular weakness, a C‑loop toric combined with a CTR implantation may be wiser. When astigmatism is high, consider a frosted‑haptic design for that extra grip.
When to add a Capsular Tension Ring
Key indications include:
- High myopia (axial length > 26 mm) – the bag stretches more.
- Pseudo‑exfoliation syndrome.
- Previous capsular complications or traumatic cataract.
Adding a CTR can transform a floppy bag into a sturdy vault, dramatically improving cataract surgery outcomes.
Post‑operative checks
- Day‑1 slit‑lamp exam to confirm centration.
- One‑week and one‑month photographs; many surgeons use image‑analysis software (see Sandoval et al., 2020) to measure rotation to within a degree.
- Advise patients to avoid vigorous eye rubbing for the first two weeks – even a small shove can shift the lens.
Bottom Line Takeaways
Intraocular lens stability is the cornerstone of successful cataract and refractive surgery. Proper pre‑op planning, picking a lens with proven haptic design, and using a capsular tension ring when zonules are weak keep the lens centered and prevent rotation that would otherwise blur vision.
Current evidence—from systematic reviews to real‑world post‑market studies—shows that modern toric and EDOF lenses rotate less than 5° in the overwhelming majority of cases, and that adding a CTR can improve stability by up to 30 % in vulnerable eyes. Follow your surgeon’s post‑op schedule, report any sudden visual changes, and you’ll enjoy lasting, crystal‑clear sight.
If you’re curious about how these concepts apply to your own eye health, feel free to explore more on IOL stability or reach out to your eye‑care professional. We’re all in this journey together, and a stable lens means a clearer view of the world—and all the beautiful moments it holds.
























Leave a Reply
You must be logged in to post a comment.