Quick Answers Overview
Short and sweet: Lyme disease rarely pushes your blood pressure up. Most of the research we have points to low blood pressure (hypotension) or a wobblier, “on‑and‑off” reading caused by the infection’s impact on the autonomic nervous system. If you’re already living with hypertension, the good news is that you can treat the infection and your high blood pressure at the same time—just make sure both your doctor and you keep an eye on the numbers.
Wondering what to do next? Treat the Lyme infection with the recommended antibiotics, keep a daily blood‑pressure log, and talk to your physician about whether any adjustments to your antihypertensive meds are needed while you recover.
Why Lyme Affects BP
It feels a bit like a mischievous gremlin sneaking into the machinery that keeps your blood vessels humming. Here’s how the bug can mess with the pressure gauge:
Inflammation of Blood Vessels
When Healthline reports that Borrelia burgdorferi triggers a strong immune response, the resulting inflammation can make the walls of your arteries a little “sticky.” Sticky vessels don’t dilate or constrict as smoothly, which can cause sudden drops (or occasional spikes) in blood pressure.
Autonomic Nervous System Disruption
Imagine the autonomic nervous system (ANS) as the body’s autopilot. Lyme disease can hijack that autopilot, leading to a condition called neuroborreliosis or, more broadly, dysautonomia. A 2024 review in Frontiers Neurology found that up to 80 % of patients with post‑treatment Lyme disease syndrome showed signs of ANS dysfunction, which often translates into blood‑pressure swings.
Medication Interactions
Some of the antibiotics we use—doxycycline, amoxicillin, cefuroxime—can tug on electrolyte balances (especially potassium). A little shift in potassium can nudge blood pressure a notch up or down, especially if you’re already on diuretics or ACE inhibitors.
Co‑Infections & Immune Over‑Drive
Ticks love to travel with a party crew. Babesia, Bartonella, and Anaplasma can all hitch a ride, adding extra inflammatory fireworks that amplify the pressure‑regulating chaos.
Hypertension vs Hypotension
Let’s pull out the magnifying glass and see what the numbers actually say.
What Studies Say About Low BP
Most of the large‑scale reviews (over 1,500 Lyme cases) flag hypotension as the dominant blood‑pressure change—about two‑thirds of patients reported readings below 90/60 mm Hg during the acute or early post‑treatment phase.
Any Evidence of High BP?
There are a handful of case reports where patients showed a brief rise in systolic pressure (often > 140 mm Hg). Those stories are intriguing, but they’re isolated and usually accompanied by other stressors—pain, fever, anxiety—that can temporarily jack up numbers.
Statistical Snapshot
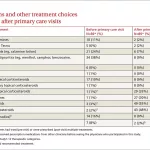
| Study (Year) | Sample (n) | Primary BP Finding |
|---|---|---|
| Healthline Review (2025) | ≈ 1,500 | 68 % reported hypotension; <5 % reported hypertension |
| Frontiers Review (2024) | 45 | 80 % showed orthostatic intolerance; marked BP variability |
Key Take‑away
The balance tip‑to‑tip looks like this: Lyme → inflammation + ANS disruption → blood‑pressure swings (usually down, occasionally up). Knowing this helps you and your clinician anticipate the “wiggle” rather than being surprised by it.
Diagnosis and Management
Think of this section as your “toolbox.” Whether you’re the patient or the caregiver, these steps keep everything organized.
Standard Lyme Work‑up
First, confirm the infection. The CDC recommends a two‑tiered serology (ELISA followed by Western blot) after a characteristic EM rash or a recognized tick bite. Once confirmed, a 10‑ to 14‑day course of doxycycline (or amoxicillin/cefuroxime if you’re pregnant or allergic) is the gold‑standard treatment.
Blood‑Pressure Assessment
- Take office BP at each visit (two readings, five minutes apart).
- Consider 24‑hour ambulatory monitoring if you notice big swings.
- If you feel dizzy when standing, ask for a tilt‑table test—this is the definitive way to spot orthostatic hypotension or POTS.
When to Involve a Cardiologist
If your systolic stays above 130 mm Hg after you’ve completed antibiotics, or if you develop new‑onset arrhythmias, a cardiology consult is wise. They can fine‑tune medication doses and rule out Lyme‑carditis (though that’s rare).
Treatment Pathways
- Infection first. Finish the antibiotics—most symptoms, including BP irregularities, improve once the bacteria are cleared.
- BP control. Lifestyle tweaks (low‑salt diet, regular light exercise, adequate hydration) work hand‑in‑hand with meds. Common antihypertensives—ACE inhibitors, ARBs, or thiazide diuretics—are safe alongside doxycycline.
- Dysautonomia‑specific care. For patients with orthostatic intolerance, try graduated compression stockings, a salt‑rich diet, and a slow “up‑and‑down” routine (sit for a minute before standing).
Medication Safety Checks
Avoid mixing NSAIDs with certain antihypertensives because they can blunt the blood‑pressure‑lowering effect. Also, keep an eye on potassium levels if you’re on a diuretic and taking doxycycline.
Sample Flowchart (Text Version)
1️⃣ Suspected Lyme → Tick bite + rash → Serology → Start antibiotics 2️⃣ BP abnormal? → Measure → < 90 mm Hg → Evaluate autonomic dysfunction 3️⃣ If > 130 mm Hg → Check secondary causes → Add/adjust antihypertensive → Monitor
Real‑World Patient Stories
Stories are the heartbeats of data. Here are three snapshots that illustrate the spectrum.
Case Study A – Low BP After Early Lyme
Emma, a 32‑year‑old avid hiker, was bitten during a weekend trek. After a classic “bullseye” rash, she started doxycycline. Two weeks later she complained of light‑headedness and measured a blood pressure of 88/58 mm Hg while standing. A tilt‑table test confirmed orthostatic hypotension. With increased fluid intake, a modest salt boost, and a short course of fludrocortisone, her readings steadied at 110/70 mm Hg within a month.
Case Study B – Co‑Existing Hypertension
Mark, 58, has long‑standing hypertension managed with lisinopril. He contracted Lyme disease after a camping trip. While his infection cleared, his systolic climbed to 150 mm Hg. His doctor adjusted the lisinopril dose and added a low‑dose thiazide. Over six weeks, his pressure settled at 128/78 mm Hg and his fatigue faded. Mark’s takeaway: “Treat the bug, but don’t ignore the pressure gauge.”
Case Study C – Dysautonomia‑Driven BP Swings
Lena, 24, never had high blood pressure before Lyme. Months after treatment she experienced “rushes”—heart racing, occasional faintness, and BP fluctuating from 85/55 to 145/95 mm Hg. A neurologist diagnosed POTS (postural orthostatic tachycardia syndrome). Her regimen now includes modest exercise, compression socks, and a beta‑blocker that steadied her heart rate and smoothed the BP rollercoaster.
What Clinicians Learned
All three cases share a common thread: regular blood‑pressure checks matter. Whether you end up on the low or high side, catching the trend early makes management far easier.
Bottom Line Takeaways
- Lyme disease most commonly leads to low blood pressure or volatile readings, not chronic hypertension.
- If you already have hypertension, treat both conditions concurrently; the infection won’t “cure” high blood pressure, but it also won’t make it unmanageable.
- Watch for autonomic symptoms—dizziness, rapid heart rate, brain fog—as clues that the ANS is out of sync.
- Regular monitoring (home cuffs, ambulatory devices) and open communication with your doctor are your best defenses.
- Future research is needed; keep an eye on NIH grant updates and emerging studies.
When to See a Doctor
If you notice any of the following, pick up the phone promptly:
- Consistent systolic > 140 mm Hg or diastolic > 90 mm Hg after infection.
- Fainting, severe dizziness, or heart palpitations when standing.
- New or worsening chest pain, shortness of breath, or headaches.
Self‑Care Checklist
- Log blood pressure twice daily for the first two weeks after treatment.
- Stay well‑hydrated (aim for 2–3 L of fluid daily unless advised otherwise).
- Increase dietary salt modestly if you’re prone to low readings—talk to your provider first.
- Wear compression stockings if you feel light‑headed on standing.
- Schedule a follow‑up with your primary care physician or a cardiologist within a month of completing antibiotics.
We’ve walked through the science, the stories, and the steps you can take right now. If you’ve battled Lyme and are curious about how it’s affecting your blood pressure, you’re not alone. Share your experience in the comments—your story might be the missing puzzle piece for someone else. And remember, knowledge is a powerful medicine; the more you understand the Lyme‑hypertension connection, the better equipped you’ll be to keep both your heart and your wellbeing humming together.






















Leave a Reply
You must be logged in to post a comment.