Hey there, friend. If you’ve ever wondered what those vague, unsettling changes in mood, focus, or social life might mean, you’re in the right place. In the next few minutes we’ll walk through the early warning signs that can show up before a full‑blown psychotic episode—what clinicians call the prodromal schizophrenia symptoms. I’ll keep it simple, sprinkle in some real‑world examples, and share the good‑news options that exist when these clues appear.
What Is Prodrome?
Definition and Timing
The word “prodrome” simply means “the first signs of something.” In psychiatry it refers to the period between the first subtle changes and the onset of full psychosis. This phase can last from a few weeks to several years, and most people who later receive a schizophrenia diagnosis have gone through it—about three‑quarters of them, according to WebMD’s overview.
Why It Matters
Spotting the prodrome isn’t about labeling someone forever; it’s about opening a door to early help that can delay—or even prevent—a full‑blown episode. Think of it like catching a small leak before a pipe bursts. Early detection gives you a chance to act, while also giving you a realistic view of the potential benefits and risks of stepping in now.
Duration Snapshot
| Typical Duration | What Studies Show |
|---|---|
| 6 months – 2 years | Most cases report a prodrome lasting this length (WebMD 2024) |
| Weeks – several months | Rapid‑onset prodromes are less common but documented in high‑risk youth (NCBI review) |
Core Early Signs
Negative‑Type Symptoms
These feel like the “quiet” side of the prodrome. You might notice:
- Social withdrawal: preferring solitude over friends, cancelling plans.
- Flat affect: reduced emotional expression, a “blank” face.
- Alogia: less speech, answering with short phrases.
These changes can be easy to miss because they creep in slowly, like a dimming light.
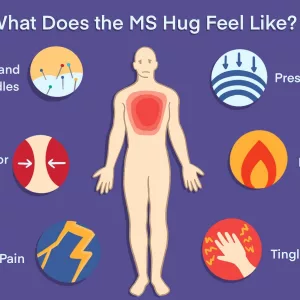
Attenuated Positive Symptoms
Now we get the “noisy” part, but it’s muted:
- Odd beliefs or mild suspiciousness—thinking that people are “watching” you more than usual.
- Subtle perceptual distortions—hearing faint whispers or seeing fleeting shadows.
- Increased anxiety or irritability without a clear trigger.
Imagine feeling a faint buzz in the background of everyday life—still noticeable, but not overwhelming.
Cognitive & Functional Shifts
These are the brain‑fog moments that often get written off as “stress”:
- Difficulty concentrating in class or at work.
- Memory lapses—misplacing keys or forgetting appointments.
- Dropping grades or declining job performance.
When these patterns stick around for weeks, they deserve a closer look.
Mood Swings & Anxiety
Feelings of sadness, irritability, or sudden panic attacks can be part of the prodrome. They’re not “just” teenage mood swings; they often come with the other signs listed above.
Quick Self‑Screen Checklist
Grab a piece of paper and tick any that feel familiar:
- ☐ I’m staying home more than before.
- ☐ My thoughts feel “fuzzy.”
- ☐ I hear faint sounds that no one else seems to notice.
- ☐ I’m unusually scared that others are judging me.
- ☐ I’ve started skipping school or work without a clear reason.
If you checked off a few, it’s worth a chat with a mental‑health professional.
Who’s At Risk?
Family History & Genetics
Having a first‑degree relative with schizophrenia bumps your risk up dramatically. Genetics alone don’t seal the fate, but they set the stage.
Early Trauma & Stress
Childhood adversity—abuse, neglect, or prolonged stress—has been linked to a higher likelihood of entering the prodrome. The brain’s stress‑response systems get rewired, making it more vulnerable.
Substance Use
Frequent cannabis use, especially in teens, amplifies the odds of experiencing early signs. Stimulants like cocaine can also tip the balance.
Neurodevelopmental Markers
Subtle motor anomalies (like clumsiness) or unusual eye‑tracking patterns sometimes appear before other symptoms. Researchers are still probing how reliable these markers are.
Risk Factor Overview
| Risk Factor | Evidence Strength |
|---|---|
| Family history of schizophrenia | High |
| Childhood trauma | Medium‑High |
| Heavy cannabis use (adolescence) | Medium |
| Early motor or sensory irregularities | Low‑Medium |
Diagnosis Process
Structured Interviews
Clinicians often use tools like the Structured Interview for Psychosis‑Risk Syndromes (SIPS) or the Comprehensive Assessment of At‑Risk Mental States (CAARMS). These interviews ask detailed questions about the frequency, intensity, and impact of the symptoms we just discussed.
Rating Scales
Two common scales are the Prodromal Questionnaire‑Brief (PQ‑B) and the Ultra‑High‑Risk (UHR) criteria. Scores above a certain threshold suggest a “clinical high‑risk” status.
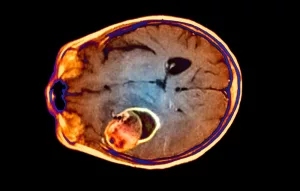
Neuroimaging & Biomarkers
Brain scans (MRI, fMRI) sometimes reveal subtle changes in gray‑matter volume or connectivity. While promising, these methods are still research‑heavy and not yet standard practice (NCBI review).
Putting It All Together
Think of diagnosis as assembling a puzzle: interview answers, questionnaire scores, family history, and any imaging data fit together to paint a picture of risk. It’s rarely a single “yes” or “no” decision.
Early Treatment Options
Low‑Dose Atypical Antipsychotics
Medications such as risperidone or aripiprazole, given at low doses, have shown modest success in delaying conversion to full psychosis. Side‑effects are generally lighter than higher doses, but weight gain, sedation, or metabolic changes can still occur.
Cognitive‑Behavioral Therapy for Psychosis (CBTp)
CBTp teaches coping skills, reality‑testing of unusual thoughts, and stress‑reduction techniques. A 2010 review highlighted that CBTp combined with medication often yields the best outcomes (Larson et al.).
Family Psychoeducation
When families learn about the prodrome, they can provide supportive environments, watch for warning signs, and reduce stigma. Many early‑intervention programs run family workshops as a core component.
Lifestyle Tweaks
Simple habits—regular sleep, balanced diet, limiting alcohol and cannabis, and stress‑management (mindfulness, gentle exercise)—can boost resilience. Think of it as fortifying the “soil” before planting anything new.
Comparison of Approaches
| Approach | Pros | Cons |
|---|---|---|
| Medication (low‑dose) | Evidence of delayed psychosis; can improve mood | Potential side‑effects; medication stigma |
| CBTp | No medication; teaches coping skills | Requires trained therapist; weekly sessions |
| Combined (med+CBT) | Best delay rates reported | Higher resource demand |
Benefits & Risks of Early Intervention
Potential Upsides
Early treatment can:
- Delay or prevent a full psychotic break in up to 30 % of high‑risk youths (Child & Adolescent Psychiatry review).
- Preserve social and academic functioning.
- Reduce long‑term medication dosage needs.
Possible Downsides
On the flip side, there are legitimate concerns:
- Medication side‑effects (weight change, sedation).
- False‑positive diagnoses—some people labeled “high risk” never develop psychosis.
- Stigma or self‑fulfilling expectations.
Shared Decision‑Making Checklist
When you sit down with a clinician, ask:
- What is the exact level of risk?
- What are the short‑ and long‑term benefits of each option?
- How will we monitor side‑effects?
- What support will my family have?
Feeling involved in the plan makes a world of difference.
Helpful Resources & Where to Get Help
National Hotlines & Directories
Organizations like NAMI (National Alliance on Mental Illness) and the Early Psychosis Intervention Network maintain state‑by‑state directories of clinics that specialize in prodrome care. A quick phone call can connect you to a local early‑intervention team.
Tracking Apps
Digital tools like MindLAMP or ePPOC let users log mood, sleep, and subtle perceptual changes. While not a diagnostic substitute, they help create a clearer picture for your provider.
Further Reading
If you want to dive deeper, consider these peer‑reviewed articles (all freely available on PubMed Central):
- Understanding the schizophrenia prodrome
- Early signs, diagnosis and therapeutics of the prodromal phase
- The prodrome and clinical risk for psychotic disorders
Conclusion
We’ve covered a lot: what the prodrome is, the subtle symptoms that can tip you off, who’s most likely to experience them, how professionals piece together a diagnosis, and the practical—and hopeful—treatment avenues that exist. The key takeaway? Early awareness empowers you to act before a crisis hits. If any of the signs resonated with you or someone you know, reach out to a trusted clinician. Early, compassionate help can make a meaningful difference in the journey.
Remember, you’re not alone in this. The mental‑health community, research workers, and families are all working toward the same goal: keeping you safe, supported, and thriving. What’s the next step for you? A conversation with your doctor? A quick self‑screen? Whatever it is, take it with confidence—you’ve got the knowledge, and you deserve the care.





















Leave a Reply
You must be logged in to post a comment.