If a breakup leaves you feeling like your heart is in pieces, imagine that same ache echoing through your skin. For many living with psoriasis, emotional pain isn’t just a fleeting mood—it can trigger real, visible flare‑ups and even affect the heart. Below you’ll find a friendly, down‑to‑earth guide that explains what those “psoriasis heartbreak symptoms” look like, why they happen, and how you can start feeling better today.
Understanding the Heartbreak
First off, let’s put a name to the feeling. “Heartbreak” in the context of psoriasis isn’t a poetic metaphor; it’s a legitimate, measurable response where stress, sadness, or grief lights up the same inflammatory pathways that cause skin plaques. In other words, the emotional and the physical are chatting with each other—sometimes loudly.
Why does this happen? Psoriasis is an autoimmune condition, meaning your immune system is a bit over‑enthusiastic. When you’re stressed, your body releases cortisol and adrenaline, which in turn can boost cytokines like IL‑17 and TNF‑α. These cytokines are the same ones that drive the rapid skin‑cell turnover you see as scaly plaques. So a broken heart can literally make the skin flare.
It’s also worth noting that chronic inflammation isn’t limited to skin. Healthline explains that the same inflammatory soup can creep into blood vessels, increasing the risk of heart disease. In short, psoriasis heartbreak symptoms can be felt on the skin, in the mind, and even in the chest.
Core Symptoms Explained
Physical Signs
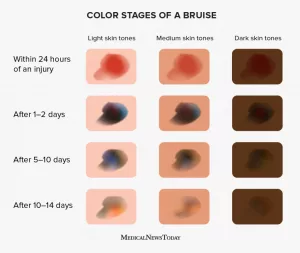
Flare‑ups after emotional triggers: You might notice new plaques forming within a day or two after an argument, a breakup, or a loss. They often appear on areas already prone to the Koebner phenomenon (where skin injury begets new lesions).
Itching and sleep disruption: The itch‑scratch cycle becomes more intense when you’re anxious or sad, leading to sleepless nights. Fatigue then feeds the mood dip—a vicious circle.
Chest tightness or palpitations: While not every person with psoriasis feels heart‑related symptoms, inflammation can make arteries stiffer. Some people notice a racing heart or a feeling of pressure after a stressful event—signs that deserve a check‑up.
Mental‑Emotional Signs
Psoriasis depression: Studies show that up to 30 % of people with severe psoriasis meet criteria for clinical depression. The constant visibility of plaques can erode self‑esteem, making it harder to bounce back from emotional blows.
Stress overload: Stress hormones amplify the IL‑17/IL‑23 pathways, essentially turning up the volume on your skin’s inflammatory soundtrack.
Social isolation: Many describe feeling “invisible” or “exposed” in social settings, leading them to withdraw. One personal story on HubPages recounts how a partner’s psoriasis made him avoid handshakes and even simple hugs—a painful reminder of how the condition can affect relationships.
Why It Happens
The science can sound intimidating, but think of it like a domino effect.
- Cytokine storm: IL‑17, IL‑23, and TNF‑α are the main messengers that cause both skin lesions and neuro‑inflammation.
- HPA‑axis dysregulation: Stress messes with the hypothalamic‑pituitary‑adrenal axis, causing spikes in cortisol that paradoxically worsen inflammation over time.
- Vascular inflammation: The same cytokines stiffen blood‑vessel walls, laying the groundwork for atherosclerosis—the “heartbreak” part of the title.
Here’s a quick visual that helps compare skin plaques with arterial plaques:
| Feature | Skin Plaque | Arterial Plaque |
|---|---|---|
| Location | Epidermis & dermis | Inner walls of arteries |
| Main Components | Keratinocytes, immune cells, lipids | Fatty deposits, calcium, inflammatory cells |
| Trigger | Genetic predisposition + immune over‑activity | Chronic inflammation + high LDL |
| Symptoms | Red, scaly patches; itching | Chest pain, reduced blood flow, possible heart attack |
Seeing the parallel helps remind us that caring for the skin is also caring for the heart.
Diagnosing the Symptoms
Because psoriasis heartbreak symptoms blend physical and mental health, a two‑pronged approach works best.
Screening Tools
Ask your dermatologist about the Dermatology Life Quality Index (DLQI). It’s a short questionnaire that captures how much psoriasis impacts everyday life. Pair that with the PHQ‑9, a trusted depression screener. If both scores are high, you’ve got a clear sign to dive deeper.
When to See a Specialist
Consider a dermatologist appointment if you notice:
- New plaques within 48 hours of a stressful event
- Itch that keeps you up more than two nights a week
- Persistent low mood for over two weeks
- Chest discomfort, rapid heartbeat, or shortness of breath
For the last bullet, a primary‑care or cardiology consult is essential—remember the link between psoriasis and heart disease is real.
Lab & Imaging Clues
Blood tests can flag systemic inflammation (CRP, ESR) and common heart‑risk markers (lipid panel, fasting glucose). An echocardiogram may reveal early left‑ventricular diastolic dysfunction—something that shows up in a handful of psoriasis patients (study).
Managing the Heartbreak
There’s no one‑size‑fits‑all cure, but a mix of lifestyle tweaks, medical therapy, and mental‑health support can dramatically lessen those heartbreak symptoms.
Lifestyle & Stress‑Reduction
Mind‑body therapies: Cognitive‑behavioral therapy (CBT) has been shown to reduce psoriasis severity by up to 30 % in some trials. Even a 10‑minute daily mindfulness practice can calm the HPA axis and lower cytokine levels.
Exercise: Aim for 150 minutes of moderate aerobic activity per week. Exercise not only improves cardiovascular health but also releases endorphins that counteract depressive feelings.
Medical & Dermatologic Interventions
Biologics that hit both skin and mood: IL‑17 inhibitors (like secukinumab) and IL‑23 blockers (guselkumab) have anecdotal reports of lifting mood scores alongside skin clearance. Talk to your dermatologist about whether a biologic fits your disease severity.
Treating comorbid depression: SSRIs, counseling, or a combination can break the cycle of low mood feeding skin inflammation. Never hesitate to ask for a mental‑health referral—your dermatologist will often welcome a collaborative approach.
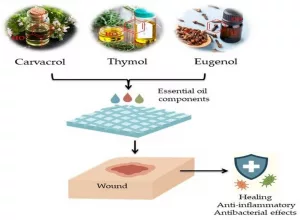
Nutrition & Supplementation
Anti‑inflammatory foods (fatty fish, walnuts, leafy greens) and omega‑3 supplements can tip the immune balance toward calm. Vitamin D, especially in people with limited sun exposure, supports skin barrier function and may modestly improve mood.
Sample 7‑Day “Heart‑Healing” Plan
- Morning: 5‑minute deep‑breathing + a glass of water with lemon.
- Mid‑day: 30‑minute walk (listen to your favorite upbeat playlist).
- Evening: Moisturise skin while watching a comedy show—laughter is a proven stress reducer.
- Nutrition: Include at least two servings of omega‑3‑rich food (salmon, chia seeds).
- Sleep: Aim for 7‑8 hours; keep the bedroom cool and screen‑free.
- Reflection: Write down one thing you’re grateful for before bed.
- Check‑in: Rate your mood and skin on a 1‑10 scale; notice patterns.
Even small, consistent steps can shrink the intensity of psoriasis heartbreak symptoms over time.
Real Patient Stories
Mike’s Break‑up Flare
Mike, 32, told me that after a three‑year relationship ended, his plaques exploded across his forearms within 48 hours. He started a biologic (ixekizumab) and simultaneously began weekly CBT. Six weeks later, his skin cleared 70 % and his PHQ‑9 score dropped from 14 (moderate depression) to 5 (minimal). He says “the therapist helped me stop replaying the breakup, and the medicine stopped my skin from yelling back.”
Laura’s Silent Sorrow
Laura, 45, never thought her “just a skin thing” could affect her heart. After years of modest flares, she experienced palpitations during a particularly stressful month at work. A cardiology echo revealed early diastolic dysfunction. Switching to a IL‑23 inhibitor and joining a local psoriasis support group gave her both physical relief and a sense of community, reducing her anxiety dramatically.
Community Resources
If you’re looking for a listening ear, the National Psoriasis Foundation runs virtual support circles and a moderated forum where members share coping tips. You can find the forum here. Connecting with others who “get it” can be a powerful antidote to heartbreak.
Final Action Checklist
- Notice emotional triggers and jot them down.
- Complete DLQI and PHQ‑9 at least once a year.
- Schedule a dermatologist review if you see rapid flare‑ups.
- Ask your primary‑care doctor about a heart‑risk assessment if you feel chest tightness or have a family history of cardiovascular disease.
- Start a simple daily stress‑relief habit (breathing, walking, or journaling).
- Consider a biologic that addresses both skin and mood—talk openly with your doctor.
- Join a support group or online community for shared experiences.
Conclusion
Psoriasis heartbreak symptoms are real, and they remind us that our bodies are wonderfully interconnected. When emotions stir up inflammation, the skin reacts, the mind feels low, and the heart may even send warning signals. By recognizing the signs, seeking the right mix of medical care, and embracing lifestyle habits that nurture both body and spirit, you can break the cycle and give yourself space to heal—inside and out. Got a story of your own, or a question about managing flare‑ups? Drop a comment below; let’s keep the conversation going and support each other on this journey.























Leave a Reply
You must be logged in to post a comment.