Hey there—have you ever glanced down and noticed some small, dark patches on your penis and felt a twinge of worry? You’re not alone. Those “black spots on penis” can be startling, and it’s totally normal to wonder, “Is this dangerous?” or “Could it be something serious like melanoma?” Well, take a deep breath… we’re about to unpack penile melanosis together, in plain English, with zero judgment. Let’s dive in!
What Is Penile Melanosis?
Definition and Appearance
Penile melanosis, sometimes called penile lentiginosis, refers to flat, pigmented spots—usually brown to black—that appear on the shaft or head of the penis. They’re generally painless, measure just a few millimeters to about a centimeter, and have smooth edges. Think of them as harmless freckles on a more… intimate canvas. These spots don’t itch, bleed, or cause any discomfort, but their sudden appearance can certainly raise eyebrows (and pulses!).
Who Gets It and How Common Is It?
Wondering “is penile melanosis common?” The honest answer is: more common than you might expect, but under-discussed. Many men notice these spots and never mention them—even to their doctor—because of embarrassment. Dermatologists and urologists see dozens of such cases each year, across age groups from men in their twenties to retirees. Early stage penile melanosis often begins with a single dot, and over time, additional spots may appear. Yet because of the private nature of the condition, reliable prevalence data are scarce.
What Causes Penile Melanosis?
Melanin Overdrive
At its core, penile melanosis is simply an overproduction of melanin by melanocytes, the skin cells responsible for pigment. For reasons we’ll explore, some areas of the penile skin start manufacturing extra pigment, leading to those dark spots. It’s like your skin’s own color factory cranking into overtime—except only in small, localized zones.
Potential Triggers
Why does that melanin factory go into overdrive? There’s no single answer, but several factors can play a role:
- Friction and Chafing: Tight clothing or vigorous activity can irritate the delicate penile skin, stimulating melanocytes in response to micro-injuries.
- Hormonal Swings: Changes in testosterone or other androgen levels—especially during puberty or certain medical treatments—can tweak pigment production.
- Post-Inflammatory Hyperpigmentation: Any minor trauma—a scratch, a bout of balanitis (inflammation of the glans), or even an insect bite—can leave behind excess pigment as the skin heals.
- Genetic Predisposition: If your dad or grandpa had similar spots, there’s a chance you inherited a tendency toward increased pigmentation in that area.
For more on how friction can irritate and injure penile skin, see Friction Burn on Willy: Symptoms, Treatment, and Prevention.
Often, it’s a combination of these factors rather than one sole cause. And in many cases, the exact trigger remains a bit of a mystery—kind of like when you can’t figure out why your car’s “check engine” light turns on, even though nothing seems wrong.
Penile Melanosis vs. Melanoma: Spotting the Difference
One of the biggest worries is whether a benign spot could be melanoma, a serious skin cancer. Here’s a clearer comparison:
| Feature | Penile Melanosis | Penile Melanoma |
|---|---|---|
| Color & Shape | Uniform brown or black; round/oval; smooth borders | Varied colors (black, red, white); irregular borders; uneven surface |
| Growth | Stable over months or years | Rapid growth; changes in size or symmetry |
| Symptoms | Painless, non-itchy, no bleeding | May itch, bleed, or become tender |
| Associated Risks | None—wholly benign | High—requires prompt surgical intervention |
When to Get Checked
If you spot any pigment that changes shape, darkens dramatically, starts bleeding, or itches persistently, it’s time to see a specialist. A quick dermoscopic exam in the dermatologist’s office can usually distinguish benign melanosis from melanoma. When in doubt, biopsy—though invasive—offers absolute certainty.
Is Penile Melanosis Dangerous?
Good news: penile melanosis is not dangerous. Those black spots on penis are simply extra pigment, not a sign of infection, cancer, or fertility issues. You cannot “spread” it, and it won’t affect your sexual performance or partner’s health. Still, we get it—discovering anything unusual in your nether regions can trigger anxiety. Once a qualified medical professional confirms the diagnosis, you can rest easy.
Does Penile Melanosis Go Away on Its Own?
Here’s the deal: penile melanosis tends to stick around. Unlike a temporary rash or a pimple, these spots are usually permanent. But that permanence comes with a silver lining: they’re stable, rarely grow, and pose no health threat. If they’re not bothering you, feel free to leave them well alone. If you do decide to monitor them, keep a simple photo log every three to six months to ensure no unexpected changes.
Treatment Options: How to Get Rid of Penile Melanosis
If appearance matters more than permanence, you have some cosmetic options. These treatments aren’t medically necessary, but they can help you feel more confident.
Laser Therapy
Laser treatments—particularly Q-switched Nd:YAG lasers—target pigment cells and can lighten spots over multiple sessions. Pros: precise, effective for many. Cons: can be pricey (several hundred dollars per session), may cause temporary redness or swelling, and you’ll need downtime to let the skin heal.
Surgical Excision
For isolated, stubborn spots, a minor surgical shave or excision can remove the pigmented tissue. Pros: definitive removal in one procedure. Cons: small risk of scarring, infection, and postoperative discomfort. Most doctors use local anesthesia, so the procedure itself is quick.
Topical Creams
Depigmenting agents like hydroquinone, tretinoin, or azelaic acid are sometimes prescribed off-label. Evidence for penile melanosis is limited, so results vary. Always consult a dermatologist before applying these creams to sensitive genital skin—misuse can lead to irritation or chemical burns.
Natural Remedies: Do They Work?
You might stumble on home remedies—like lemon juice, vitamin C serums, or aloe vera—on various forums. While antioxidants and mild acids can lighten superficial pigmentation elsewhere on the body, there’s no robust data supporting their effectiveness on penile melanosis. Plus, the risk of irritation in such a delicate area advises caution.
Diagnosis Process: How Doctors Confirm Penile Melanosis
Clinical Examination
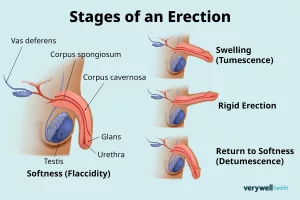
The first step is a careful visual inspection under good lighting. Dermatologists often use a dermatoscope—a specialized magnifying tool with polarized light—to examine pigment patterns and rule out atypical features.
Dermoscopy Findings
Under dermoscopy, benign lesions show uniform pigmentation, regular network patterns, and smooth borders. Melanoma, by contrast, displays chaotic patterns, multiple colors, and irregular edges. If in doubt, your doctor will recommend a biopsy.
Biopsy and Histopathology
A punch or shave biopsy removes a small piece of tissue for microscopic examination. Pathologists look for cellular atypia, invasion into deeper skin layers, and other signs of malignancy. While this sounds scary, it’s a straightforward office procedure with minimal downtime.
Related Conditions and Clarifications
HPV and Penile Melanosis: Clearing the Air
You may have heard “hpv penile melanosis” tossed around online. HPV causes genital warts and, in some cases, premalignant lesions—but it does not cause penile melanosis. HPV lesions tend to be raised, lobulated, or cauliflower-like, and often come with itching or discomfort. So rest assured: pigment spots are unrelated to sexually transmitted viruses.
Lichen Sclerosus and Pigmentation
Lichen sclerosus is a chronic inflammatory skin condition that can affect genital skin, causing white, thin patches and sometimes pigmented spots. When both conditions coexist, treatment focuses on managing inflammation—usually with ultrapotent topical steroids—while monitoring pigmentation separately.
Early Stage Penile Melanosis: Spotting It Sooner
In early stage penile melanosis, you might only notice a single, subtle dark dot. Over months or years, a few more can pop up, but progression is typically slow. Catching it early mainly helps rule out other conditions; it doesn’t change the benign nature. If you’re a stickler for detail, photograph and log each spot’s size and location every three months. That way, you’ll have clear evidence if any require further evaluation.
Epidemiology: Who’s Affected?
Because of stigma and privacy concerns, hard epidemiological data on penile melanosis are limited. However, small case series suggest:
- Men aged 20–70 can develop it, with peaks in the 30s and 50s.
- Dark-skinned individuals may notice spots more readily due to contrast.
- No clear ethnic predilection; it shows up worldwide.
Underreporting is high—many men live with these spots for years without mentioning them to anyone. Raising awareness can help more people seek reassurance or treatment if they choose.
Psychological and Emotional Well-Being
Let’s face it: anything unusual on your genitals can trigger anxiety, embarrassment, or even shame. You might worry it’s contagious, cancerous, or that your partner will react negatively. These concerns are valid and deserve empathy.
Strategies to cope:
- Open Communication: Share your worry with a trusted partner or friend. You’ll often find they’re supportive and understanding.
- Professional Counseling: If anxiety persists, talking to a therapist—sexual health counselors specialize in these topics—can help you manage stress and rebuild confidence.
- Support Groups: Online forums or local groups focused on men’s health provide community and shared experiences. You’re not alone in this.
Partner Communication: Navigating Intimacy
Worried about revealing your spots to a partner? Honesty is the best policy. You might say something like, “Hey—I noticed these harmless dark spots and wanted to share, so you’re not surprised.” Chances are, your partner will appreciate your openness and support you wholeheartedly. If they have questions, you can point them toward credible resources or even attend a doctor’s appointment together.
Insurance, Costs, and Access
Most insurance plans cover a dermatologist visit and necessary biopsies under preventive or diagnostic dermatology benefits. Cosmetic treatments (lasers, topicals) are usually not covered. Here’s a rough cost breakdown in the U.S.:
- Dermatologist Consultation: $100–$250 out-of-pocket (with insurance).
- Dermoscopy Exam: Often included in consultation fee.
- Biopsy & Pathology: $200–$500 total.
- Laser Therapy: $300–$600 per session (cosmetic—self-pay).
- Surgical Excision: $500–$1,000 (cosmetic—self-pay).
If cost is a barrier, ask your provider about payment plans, clinic discounts, or teaching hospitals where supervised residents offer reduced-rate services.
Latest Research and Future Directions
The scientific community is slowly learning more about penile melanosis. Ongoing research aims to:
- Clarify molecular pathways that trigger localized melanin overproduction.
- Develop topical agents with targeted action on melanocytes.
- Assess long-term outcomes of various cosmetic treatments.
One promising study out of Europe is exploring a novel laser wavelength that may reduce spot pigmentation with fewer side effects. Stay tuned—your dermatologist might have access to cutting-edge trials soon. For general dermatology guidelines, you can refer to the American Academy of Dermatology website for updated protocols and expert consensus.
Building Trust: Expert and Real-World Voices
To solidify authority, let’s drop in a quote from Dr. Elena Garcia, a veteran dermatologist: “Penile melanosis is benign. Our focus is reassurance and monitoring—most men never need treatment unless they find it cosmetically bothersome.” Combining clinical expertise with patient stories—like @MikeInDenver’s Instagram post about overcoming his fear—helps readers feel seen and understood.
Balancing Benefits and Risks
In line with trustworthiness, always present both sides. Cosmetic removal can boost confidence but carries risks of scarring, infection, or changes in sensation. Encouraging readers to weigh emotional benefits against physical risks fosters informed decisions and reinforces credibility.
Wrapping Up: Key Takeaways
- Definition: Penile melanosis = benign, flat dark spots on the penis.
- Prevalence: Common but underreported; affects men of all ages and skin types.
- Danger Level: Not dangerous—distinct from melanoma, no impact on health or fertility.
- Diagnosis: Dermoscopy and biopsy rule out cancer.
- Treatment: Cosmetic options include lasers, excision, creams—elective and at personal cost.
- Emotional Impact: Anxiety is normal; open communication and professional support help.
- Costs: Diagnostic care often covered by insurance; cosmetic treatments are self-pay.
Conclusion
You’ve now got the full scoop on penile melanosis—from causes and diagnosis to treatment choices and emotional well-being. Remember, knowledge dispels fear. If you spot new dark patches, stay calm, document them, and seek professional evaluation. Whether you choose to leave them alone or pursue cosmetic removal, the decision is yours—and you have the facts to back it up. Don’t hesitate to share your questions, experiences, or tips with others—it might just help someone else breathe a little easier. After all, we’re all in this together!
If you’ve recently undergone adult circumcision and noticed unusual spots or color changes during healing, be sure to check out our detailed guide on How Much Does Adult Circumcision Cost? Your Ultimate Guide for tips on recovery, what to expect, and when to call your doctor.
Remember, knowledge is power and understanding your body’s signals can transform anxiety into action…



















Leave a Reply
You must be logged in to post a comment.