Did you ever notice that a looming deadline can make your stomach feel like a rubber band about to snap? It’s not just “in your head.” Your brain and gut are in constant conversation, and stress is the loud‑speaker that can turn a friendly chat into a shouting match. In the next few minutes we’ll unpack how stress talks to your gut, why that matters for everything from digestion to mood, and—most importantly—what simple steps you can take right now to calm the whole system.
How Stress Affects Gut
Physiological pathways that link stress to digestion
When you encounter a stressor, your brain fires up the autonomic nervous system. The sympathetic branch—think “fight‑or‑flight”—releases adrenaline and revs up your heart rate. At the same time, the parasympathetic “rest‑and‑digest” branch gets pushed aside. This shift alone can change the speed at which food moves through your intestines.
Autonomic nervous system: the push‑pull switch
The gut has its own “little brain,” the enteric nervous system, packed with about 100 million nerve cells. Those cells get direct signals from the vagus nerve, the main highway connecting brain and belly. When stress dominates, the vagus nerve quiets, slowing stomach emptying and often causing that uncomfortable “butterflies” sensation.
Hormonal messengers: cortisol and adrenaline
Cortisol, the classic “stress hormone,” spikes within minutes of a stressful event. In the gut, cortisol can widen the tight junctions between cells, making the intestinal barrier more “leaky.” A leaky gut lets bacterial fragments slip through, which can trigger inflammation and even amplify the stress response—a vicious circle.
Key hormones that carry the message
One hormone that often flies under the radar is corticotropin‑releasing factor (CRF). Researchers have shown that CRF released in the brain can travel to the gut and directly stimulate colonic muscles, causing diarrhea‑type symptoms. A 2024 study in Frontiers describes how CRF‑driven inflammation may be the bridge between acute stress and chronic gut problems.
CRF‑1 vs. CRF‑2 receptors
CRF‑1 receptors tend to crank up colonic contractions, while CRF‑2 receptors slow down the upper gut. This dual action explains why stress can both speed up and slow down different parts of the digestive tract at the same time.
Stress and the gut microbiome
Even a short burst of anxiety can shift the composition of your gut bacteria—a phenomenon called dysbiosis. The Nature article from 2023 revealed that stress‑induced chemical signals from the brain cause gut nerve cells to release inflammatory messengers, which in turn disturb the microbial balance.
Why dysbiosis matters
When good bacteria dwindle, beneficial metabolites like short‑chain fatty acids (SCFAs) drop. SCFAs help keep the gut lining tight and signal the brain that everything’s fine. A loss of these “peacekeepers” can leave you feeling bloated, irritable, and even more stressed.
Gut‑Brain Axis Basics
What the gut‑brain axis really is
The gut‑brain axis (or gut‑brain connection) is a two‑way street. Signals travel from the brain to the gut via the autonomic nerves, hormones, and immune molecules, and they travel back from the gut through the vagus nerve, microbial metabolites, and even cytokines.
Bidirectional communication
Think of it as a duet: the brain writes the melody, the gut provides the rhythm, and the microbiome adds the harmony. If any instrument goes out of tune, the whole song suffers.
How microbes join the conversation
More than 90 % of the body’s serotonin—often called the “feel‑good” neurotransmitter—is produced in the gut. This serotonin doesn’t cross the blood‑brain barrier, but it influences the vagus nerve and immune cells, subtly shaping mood and anxiety.
According to a Harvard Health article on the gut‑brain axis, the microbiome can affect brain function by releasing neurotransmitter‑like compounds, modulating inflammation, and even tweaking the blood‑brain barrier.
Short‑chain fatty acids and brain health
SCFAs such as butyrate act like tiny diplomats, calming inflammation in both gut and brain. When stress reduces SCFA production, you may notice heightened anxiety and a “foggy” mind.
When the gut talks back to the brain
Gut inflammation can send distress signals up the vagus nerve, waking up brain regions that process pain and emotion. That’s why people with chronic inflammatory bowel disease often report anxiety or depression, even when the “outside world” feels calm.
Real‑world example
Take Maya, a freelance graphic designer. During a high‑stress client project, her IBS flared, and she started feeling panicky even after the deadline passed. By the time she consulted a gastroenterologist, she learned that her gut inflammation was amplifying her stress hormones. After introducing a low‑FODMAP diet and a daily 5‑minute breathing routine, her anxiety and gut pain both eased.
Stress Gut Signs
Acute symptoms you can spot instantly
Ever felt “butterflies” before a presentation? That’s a classic stress‑digestion response. Common acute signs include:
- Nausea or an upset stomach
- Quick, cramping pain in the lower abdomen
- Sudden urgency to use the bathroom
Why these happen
Quick releases of adrenaline divert blood away from the digestive tract, slowing digestion and causing that queasy feeling. At the same time, the brain may trigger a surge of gastric acid as a defensive measure, leading to heartburn.
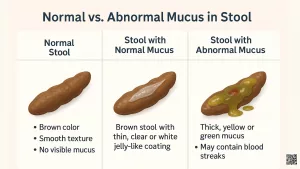
Chronic patterns that hint at a stress‑gut loop
If you notice any of the following for weeks or months, stress might be the hidden culprit:
- Alternating diarrhea and constipation
- Persistent bloating despite a “healthy” diet
- Frequent abdominal pain that improves when you relax
Quick self‑check
Answer these five questions honestly:
- Do you often feel tension in your chest or neck before meals?
- Do you experience stomach pain after a stressful meeting?
- Does anxiety make you crave sugary or greasy foods?
- Have you noticed changes in your stool consistency during stressful periods?
- Do you feel better after a short walk or breathing exercise?
If you answered “yes” to three or more, it’s worth exploring stress‑reduction strategies.
Calm Your Gut
Lifestyle tweaks that lower cortisol fast
Here are three actions you can start doing right now—no fancy equipment required:
- 5‑minute diaphragmatic breathing: Inhale through the nose for a count of four, let your belly rise, then exhale slowly for a count of six. Repeat five times. Studies show this drops cortisol within minutes.
- Short nature walks: A 10‑minute walk outdoors can reduce sympathetic activity and boost parasympathetic tone, improving gut motility.
- Progressive muscle relaxation: Tense each muscle group for three seconds, then release. It’s especially helpful before bedtime to prevent nighttime gut flare‑ups.
Science behind it
A 2023 Harvard Health guide on stress‑reduction notes that breathwork and gentle movement activate the vagus nerve, directly calming the gut‑brain axis.
Dietary habits that protect gut health under stress
Food is both fuel and messenger. When stress levels rise, choose foods that nurture the microbiome and keep the gut lining sturdy.
Low‑FODMAP basics
FODMAPs are short‑chain carbs that ferment quickly, causing bloating and gas—symptoms that intensify under stress. A low‑FODMAP diet (temporarily) can reduce those uncomfortable episodes.
Fermented foods and prebiotic fiber
Yogurt, kefir, sauerkraut, and kimchi supply live cultures that repopulate good bacteria. Pair them with prebiotic fibers like chicory root, onions, or bananas to feed those microbes.
Probiotics and supplements that help
Not all probiotics are created equal. Research points to a few strains that specifically blunt stress‑induced gut inflammation:
- Lactobacillus rhamnosus GG – shown to reduce cortisol and improve IBS symptoms.
- Bifidobacterium longum – helps maintain barrier integrity.
- Vitamin D – supports immune regulation, potentially lowering gut inflammation.
When to seek professional help
If you experience any of the following, it’s time to call a doctor:
- Unexplained weight loss
- Blood in stool
- Severe, persistent abdominal pain
- Symptoms that linger despite lifestyle changes for more than three weeks
Both a gastroenterologist and a mental‑health professional can work together to break the stress‑gut cycle.
7‑Day Stress‑Gut Reset Plan
Ready for a practical roadmap? Follow this one‑week plan. Each day builds on the previous one, so you’ll feel a gradual lift in both mood and digestion.
| Day | Action | Time Needed | Gut Benefit |
|---|---|---|---|
| 1 | Morning 5‑minute diaphragmatic breathing | 5 min | Lowers cortisol, activates vagus nerve |
| 2 | Add a cup of kefir to breakfast | — | Introduces live probiotics |
| 3 | 30‑minute brisk walk after lunch | 30 min | Improves intestinal motility |
| 4 | Low‑FODMAP dinner (e.g., zucchini noodles with basil pesto) | — | Reduces bloating and gas |
| 5 | Evening journaling: note stress triggers & gut reactions | 10 min | Increases self‑awareness, guides future tweaks |
| 6 | Gentle “belly‑friendly” yoga flow | 20 min | Boosts parasympathetic tone |
| 7 | Review the week & plan next steps | 15 min | Solidifies habit loop |
Feel free to swap activities that don’t fit your schedule—consistency matters more than perfection.
Putting It All Together
We’ve traveled from the microscopic world of CRF hormones all the way to a friendly 7‑day plan you can start tonight. The key takeaways?
- Stress and the gut speak a common language of hormones, nerves, and microbes.
- Even short bursts of anxiety can loosen the gut barrier, alter your microbiome, and trigger uncomfortable symptoms.
- Simple, evidence‑based habits—breathing, movement, mindful eating, and targeted probiotics—can calm that conversation.
- If symptoms persist, professional guidance is essential; you deserve a gut that feels as steady as your best friend.
Now it’s your turn. Which of the reset steps will you try first? Have you noticed a particular food or habit that makes stress flare up your stomach? Share your story in the comments below or drop a question—let’s keep the conversation going. Your gut will thank you, and you’ll be one step closer to a calmer mind, a happier belly, and a life where stress doesn’t call the shots.



















Leave a Reply
You must be logged in to post a comment.