Quick answer: Treating ADHD (TDAH) usually means mixing medicines, therapy, and sometimes natural tricks. The best combo depends on how old you are, how strong the symptoms are, and what fits your daily life.
Quick answer 2: Knowing the ups and downs of each option lets you build a balanced plan that sharpens focus, tames impulsivity, and keeps your health safe.
What Treatment Covers
When we talk about tratamiento TDAH, we’re not just talking about popping a pill. Think of it as a toolbox. Inside you’ll find:
- Medication to adjust brain chemistry.
- Therapy that reshapes habits and thoughts.
- Lifestyle tweaks – exercise, sleep, diet, mindfulness.
- School or workplace accommodations.
- Sometimes, evidence‑based natural supplements.
Why a multimodal approach? According to the CDC, most people see the biggest gains when medication and behavioral therapy are used together. The brain is a complex orchestra; you need more than a single instrument to keep the music in tune.
Why Mix Strategies?
ADHD affects attention, impulsivity, and hyperactivity – three different conductors. Medication can quiet the “noise” but therapy teaches you how to read the score. Lifestyle moves the tempo so you don’t get out of sync. Think of it like training for a marathon: you need shoes (meds), a training plan (therapy), and proper nutrition (lifestyle) to finish strong.
Factors That Shape Your Choice
Before you pick a path, ask yourself:
- What’s my age or my child’s age?
- Do we have co‑occurring conditions (anxiety, depression, learning disorders)?
- How supportive is my home, school, or work environment?
- What are my personal preferences or cultural values?
These answers guide whether you start with therapy, medication, or a blend of both.
Medication Basics Overview
Medicamentos TDAH are often the first thing people think of. They aren’t magic bullets, but they’re powerful tools when used wisely.
Stimulant Meds
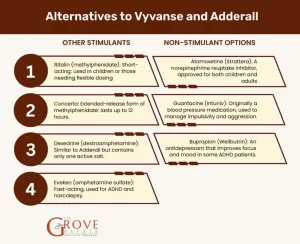
Stimulants such as methylphenidate (Ritalin, Concerta) and amphetamine‑based drugs (Adderall, Vyvanse) boost dopamine and norepinephrine, essentially “turning up the volume” on the brain’s focus center. Most research, including a review on Healthline, shows they improve attention in 70‑80 % of users.
Pros & Cons
| Pros | Cons |
|---|---|
| Fast symptom relief (often within 30‑60 min) | Potential side‑effects: insomnia, appetite loss, irritability |
| Well‑studied, many dosage forms (short‑, intermediate‑, long‑acting) | Risk of misuse or diversion, especially in teens |
| Can be combined with behavioral therapy for greater gains | May not be suitable for kids with certain heart conditions |
Non‑Stimulant Options
When stimulants aren’t tolerated, doctors may turn to atomoxetine (Strattera), guanfacine (Intuniv), or extended‑release clonidine (Kapvay). These work slower but avoid many of the “buzz” side‑effects.
When to Choose Non‑Stimulants
- History of anxiety or tic disorders.
- Concerns about misuse (college students, adults with substance‑use history).
- Need for a once‑daily dose that lasts into the evening.
Starting & Tuning the Dose
First, a thorough medical exam and a detailed symptom rating (often the DSM‑5 checklist) are required. The doctor will begin with a low dose, monitor response for 1–2 weeks, then adjust upward as needed. Keep a simple log: medication name, dose, time, and any side‑effects you notice.
Red Flags to Watch
If you see any of the following, call your provider right away:
- Severe mood swings or new depressive thoughts.
- Chest pain, rapid heartbeat, or high blood pressure.
- Unusual tics or tremors.
- Signs of misuse (feeling “high,” craving the pill).
Therapy Options Explained
Medication can calm the storm, but therapy builds the shelter.
Behavioral Therapy for Kids
The American Academy of Pediatrics (AAP) recommends that for children under six, parent‑training in behavior management should be the first line of treatment. Think of it as giving parents a “coach’s playbook” to handle tantrums, improve routine, and reinforce positive actions.
Key Techniques
- Positive reinforcement: reward a desired behavior immediately (stickers, extra playtime).
- Clear expectations: visual schedules help kids know what’s coming next.
- Consistent consequences: a predictable system reduces confusion.
Cognitive‑Behavioral Therapy (CBT) for Teens & Adults
CBT tackles the “thinking” side of ADHD. It teaches you to spot automatic thoughts that lead to procrastination, then replace them with actionable plans. A typical session might look like:
- Identify a problem (e.g., “I can’t start my report”).
- Break it into tiny steps (open laptop → outline → write 100 words).
- Use timers or the Pomodoro technique to stay on track.
- Review what worked and tweak what didn’t.
School & Workplace Supports
Getting a 504 Plan or Individualized Education Program (IEP) can provide accommodations such as extended test time, preferential seating, or a quiet workspace. Talk to teachers, counselors, or HR early – they often want to help, they just need a clear request.
Executive‑Function Coaching
Coaches work one‑on‑one to build skills like time‑management, organization, and self‑advocacy. Unlike therapy, coaching is future‑focused and goal‑oriented. Many adults with TDAH report a “light‑switch” moment when they finally learn to structure their day.
Natural Alternatives Guide
“Alternativas naturales TDAH” are tempting, but the evidence is mixed. Let’s separate hype from science.
Omega‑3 Fatty Acids
Fish oil supplements (EPA/DHA) have shown modest improvements in attention in several trials. The CDC notes that the data isn’t strong enough to replace medication, but they’re low‑risk and can support brain health.
Dietary Tweaks
Reducing added sugars and artificial food colorings might help some children, especially those who are sensitive. However, a systematic review from AHRQ (2023) found no consistent benefit across large populations.
Exercise & Mindfulness
Regular aerobic activity releases dopamine and norepinephrine naturally – essentially a “natural stimulant.” A 30‑minute brisk walk or a short dance break can boost focus for the next hour. Mindfulness meditation, even just five minutes a day, has been linked to lower impulsivity scores.
Biofeedback & Neurofeedback
These technologies train you to control brainwave patterns through visual or auditory cues. Some studies report improvement, but the cost and limited insurance coverage keep them from mainstream use.
Bottom Line on Naturals
Think of natural options as complementary allies, not stand‑alone cures. Discuss any supplement with your doctor – some can interact with stimulant meds (e.g., high‑dose caffeine).
Treatment By Age
Age matters because the brain, responsibilities, and support systems evolve.
Kids (0‑12 Years)
Early years focus on behavior training, school accommodations, and, when symptoms are moderate‑to‑severe, medication. The AAP suggests starting with parent training before meds for kids under six, then combining both after age six.
Teens (13‑17 Years)
Adolescents often juggle school, extracurriculars, and emerging independence. A blend of stimulant medication, CBT, and a structured academic plan works well. Involve the teen in decision‑making to boost adherence.
Adults
Adults with TDAH may face job performance, relationship, or financial challenges. Treatment typically includes medication (stimulants or non‑stimulants), executive‑function coaching, and therapy that addresses emotional regulation.
According to Mayo Clinic, the best outcomes arise when medication is paired with skills training and counseling.
Building Your Plan
Creating a treatment plan is a bit like planning a road trip. You need a destination, a map, and checkpoints.
Step 1: Set Measurable Goals
Pick 3‑5 concrete outcomes you can track. Examples:
- Finish homework without prompts at least 4 out of 5 evenings.
- Arrive on time for work meetings 90 % of the time.
- Reduce “interrupting” comments in conversations from 8 times/day to 2.
Step 2: Assemble Your Team
Typical members include:
- Primary care doctor or pediatrician.
- Psychiatrist or neurologist (prescribes meds).
- Therapist or psychologist (CBT, behavior therapy).
- School counselor or special‑education coordinator.
- Coach or trusted adult for executive‑function support.
Step 3: Schedule Regular Check‑Ins
First review at one month, then at three months, and every six months thereafter. Use a simple rating scale (0‑3) for each goal and adjust meds or strategies accordingly.
Step 4: Keep a Simple Log
Best practice: a notebook or phone note with columns – Date | Medication Dose | Mood/Side Effects | Goal Progress. Review it with your clinician before each appointment.
Resources and Authority
Reliable sources make your journey smoother. Here are a few you can trust:
- CDC – offers up‑to‑date treatment guidelines and age‑specific recommendations.
- Mayo Clinic – comprehensive overviews for adults and children.
- CHADD (Children and Adults with Attention‑Deficit/Hyperactivity Disorder) – community support, webinars, and parenting tips.
- AHRQ systematic review (2023) – deep dive into medication efficacy and natural adjuncts.
Remember, the best plan is the one you feel comfortable following and that shows real progress over time.
Conclusion
Whether you’re a parent navigating a child’s diagnosis, a teen figuring out how to stay on top of schoolwork, or an adult seeking focus at work, treating ADHD is a personalized adventure. By blending medication, therapy, lifestyle tweaks, and evidence‑based natural options, you can craft a plan that respects both the benefits and the risks. Keep your goals clear, lean on a supportive team, and stay curious about what works best for you.
What’s worked for you? Have you tried a new strategy that made a difference? Share your story in the comments – your experience could be the bright idea another reader needs.





















Leave a Reply
You must be logged in to post a comment.