Short answer: yes, the microbes living in your gut can push you toward or pull you away from colon cancer. And the good news? Simple changes to your diet, lifestyle, and even medical‑grade microbiome tweaks can tip the balance in your favor.
In the next 15‑20 minutes we’ll walk through what the science says, why it matters to you, and how you can take practical steps right now. Grab a cup of tea, settle in, and let’s talk gut bacteria and colon cancer like old friends.
Gut Bacteria Impact
Dysbiosis vs Eubiosis
Think of your gut as a bustling city. When the neighborhoods are tidy, the streets clean, and the residents get along – that’s eubiosis. But when the city’s trash piles up, gangs take over, and fires break out – that’s dysbiosis. In the gut, dysbiosis means an imbalance of microbes that fuels inflammation, produces harmful metabolites, and ultimately can damage the DNA of colon cells.
According to a 2023 review, dysbiosis is a key risk factor for colorectal cancer Liu et al.. The authors explain that an excess of pro‑inflammatory bacteria can trigger a cascade of molecular events that turn normal cells into tumor‑seeded cells.
Key Bacterial Players
Not all bacteria are villains. Some are protective, while others act like mischievous trouble‑makers:
- Fusobacterium nucleatum – loves to stick to colon cells and hijack the immune system, promoting tumor growth.
- Enterotoxigenic Bacteroides fragilis – releases a toxin that triggers chronic inflammation.
- Lactococcus – often associated with a healthier gut, can produce beneficial short‑chain fatty acids (SCFAs).
- Escherichia‑Shigella – elevated levels are linked with higher cancer risk.
A 2021 study found that patients with colorectal cancer had higher Fusobacteria and lower Proteobacteria compared with healthy volunteers Gao et al.. Those shifts aren’t random; they reflect a gut environment that’s becoming more conducive to tumor development.
Mechanistic Pathways
How do these microbes actually cause trouble? Three main routes:
- Metabolites – Harmful metabolites like secondary bile acids can irritate the colon lining, while protective metabolites like butyrate help keep cells healthy.
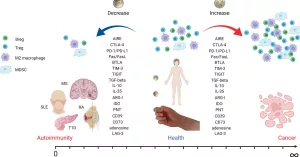
- Immune Modulation – Certain bacteria interact with micro‑RNA (miRNA) in colon cells, messing with gene expression and immune surveillance. A 2025 Frontiers review highlights how gut microbes shape tumor‑immune responses.
- Inflammation – Persistent low‑grade inflammation creates a fertile ground for DNA mutations to stick around and proliferate.
Early Detection Tools
Stool‑Based Biomarkers
Imagine a home‑test kit that not only checks for hidden blood but also reads the DNA of the bacteria living in your poop. That’s where stool‑based microbiome panels come in. By sequencing the 16S rRNA gene, labs can generate a “risk score” that flags an elevated likelihood of advanced adenomas or early‑stage cancer. In pilot studies, these scores achieved around 78 % sensitivity for detecting lesions larger than 10 mm.
Tissue‑Level Signatures
When doctors take a colon biopsy, they also get a glimpse of the mucosa‑associated microbes. Research shows that cancerous tissue often hosts a distinct microbial community compared with adjacent normal tissue. A 2016 Genes & Environment article reported that Fusobacterium and Lactococcus abundance differed significantly between tumor and non‑tumor sites Yamamoto & Matsumoto. Combining these tissue signatures with histopathology may sharpen diagnostic precision.
Clinical Utility
Right now, most gastroenterologists rely on colonoscopy for definitive diagnosis, but microbiome data is creeping into risk‑stratification algorithms. A few ongoing clinical trials are testing whether a high‑risk microbiome profile can trigger earlier colonoscopy scheduling. Keep an eye on the news; the next few years could bring FDA‑approved microbiome‑based screening tools.
Real‑World Example
Consider Jane, a 52‑year‑old who loved sushi and ran marathons. She felt perfectly healthy, but her doctor suggested a stool‑based microbiome test after a family history of CRC. The test flagged an elevated risk score, prompting a colonoscopy that caught a small, easily removable polyp. Jane’s story shows how a simple microbial snapshot can catch trouble before it becomes serious.
Treatment Response
Impact on Chemotherapy
Ever heard of “chemo‑resistant” tumors? Some gut bacteria actually break down chemotherapy drugs before they reach the tumor. Fusobacterium species have been shown to metabolize 5‑fluorouracil (5‑FU), dulling its effectiveness. The 2023 Liu et al. review notes a clear link between high Fusobacterium load and poorer response to standard CRC regimens.
Impact on Immunotherapy
Immunotherapy is a game‑changer for many cancers, but its success in colorectal cancer hinges on the gut’s microbial makeup. A 2025 Frontiers review highlighted that patients whose stools were enriched with Bifidobacterium and Faecalibacterium responded far better to PD‑1 inhibitors. In one small trial, a fecal microbiota transplant (FMT) from a responder turned a non‑responder into a responder within weeks.
Modulation Strategies
So, can we “re‑program” the gut to help our treatments? Here are three evidence‑backed options:
- Probiotics – Strains like Lactobacillus rhamnosus and Bifidobacterium longum have shown promise in pre‑clinical models for boosting chemo efficacy.
- Prebiotics – Foods high in inulin or resistant starch feed beneficial bacteria, increasing SCFA production.
- FMT – Transferring stool from a screened, healthy donor can reshape the recipient’s microbiome. Safety protocols are strict, but early data are encouraging for CRC patients undergoing immunotherapy.
Practical Checklist
- Talk to your oncologist about stool‑based microbiome testing.
- If you’re on chemo, ask whether a probiotic regimen could help.
- Consider a high‑fiber, plant‑rich diet to support beneficial microbes.
- Only pursue FMT under a clinical trial or specialist supervision.
Diet & Prevention
Foods That Feed Protective Bacteria
Think of fiber as the fertilizer for your gut garden. Whole grains, beans, legumes, fruits, and veggies ferment into butyrate—a SCFA that fuels colon cells and blocks inflammation. Fermented gems like yogurt, kefir, kimchi, and sauerkraut are natural probiotic boosters, delivering live Lactobacillus and Bifidobacterium straight to the colon.
Foods That Promote Dysbiosis
On the flip side, red and processed meats, high‑fat dairy, and sugary drinks tend to nourish harmful bacteria like Fusobacterium and Bacteroides fragilis. A diet heavy in these foods can raise secondary bile acid levels, which are known tumor promoters.
Evidence‑Based Diet Plans
Multiple cohort studies agree: the Mediterranean diet—rich in olive oil, fish, nuts, fruits, and vegetables—lowers colorectal cancer incidence by up to 30 %. One randomized trial gave participants a 7‑day “Gut‑Health Meal Plan” packed with 30 g of fiber daily, and after three months, stool analyses showed a 20 % increase in butyrate‑producing bacteria.
Supplement Caution
Not all probiotic pills are created equal. Look for products that list specific strains (e.g., Lactobacillus acidophilus LA‑5) and have been tested in clinical trials. Over‑supplementation, especially for immunocompromised patients, can sometimes cause infections. As always, check with your doctor before adding a new supplement.
Risk & Safety
When Microbiome Tweaks Can Backfire
Changing the gut isn’t without risk. Broad‑spectrum antibiotics can wipe out beneficial microbes, paving the way for opportunistic pathogens. Unscreened FMT carries a small but real chance of transmitting infections or unwanted antibiotic‑resistance genes.
Regulatory Landscape
The FDA currently treats FMT as an investigational new drug (IND) when used for anything beyond recurrent C. diff. infection. That means any clinic offering FMT for cancer must adhere to strict donor‑screening standards and obtain proper regulatory clearance.
Decision‑Making Flowchart
| Question | Yes | No |
|---|---|---|
| Do you have a high colon‑cancer risk (family history, age > 50, etc.)? | Proceed to stool‑based microbiome testing. | Maintain a balanced gut‑health diet. |
| Did the test show dysbiosis or high‑risk bacteria? | Discuss probiotic/prebiotic plan with your doctor. | Continue regular screening (colonoscopy). |
| Are you undergoing chemotherapy or immunotherapy? | Ask about microbiome‑modulating adjuncts. | Standard cancer care pathway. |
| Is FMT being considered? | Only under a clinical trial with FDA oversight. | Skip FMT; focus on diet & lifestyle. |
Takeaway & Action
Bottom line: your gut microbiome is a double‑edged sword. Certain bacteria can whisper “grow” to rogue colon cells, while a thriving community of friendly microbes shouts “stay healthy.” By understanding which microbes are allies and which are adversaries, you gain a new lever to lower colon‑cancer risk and improve treatment outcomes.
Here’s a quick action plan you can start today:
- Get evaluated. If you’re over 50 or have a family history, ask your doctor about a stool‑based microbiome risk test.
- Eat for your microbes. Fill half your plate with colorful, fiber‑rich plant foods and add a daily serving of fermented foods.
- Mind the meds. Avoid unnecessary antibiotics; discuss probiotic options if you’re on chemo.
- Stay informed. New microbiome‑based screening tools are on the horizon—follow reputable health news and ask your provider about clinical trials.
We’ve covered a lot, but the conversation doesn’t have to end here. If you have questions about your own gut health, or want to share a success story, drop a comment below. Let’s keep learning from each other—and keep those gut bacteria on our side!






















Leave a Reply
You must be logged in to post a comment.