Hey there! If you’ve ever wondered whether the dreaded “appendix attack” runs in families, you’re not alone. The short answer is: appendicitis isn’t a classic hereditary disease, but having a close relative who’s dealt with it can raise your odds a bit. Knowing the science, the lifestyle pieces, and the practical steps you can take today helps you stay ahead of the pain—and maybe even keep that little pouch from bothering you at all.
What Hereditary Means
Let’s start with definitions—because the words “hereditary” and “genetic” get tossed around like confetti at a party, and they’re not the same thing.
Hereditary describes traits that are passed directly from parent to child through a single gene or a set of genes, like eye color or certain rare diseases. Genetic predisposition, on the other hand, means you might carry variations that make you a little more susceptible, but other factors (diet, infections, plain luck) decide whether the condition actually shows up.
In the world of appendicitis, most researchers agree we’re looking at a genetic influence rather than a true hereditary pattern. As Healthline explains, the condition isn’t inherited the way cystic fibrosis is, but certain gene variations may nudge the odds upward.
Family History Risk
So, what does the data say about family history?
- A 2012 study in the Western Journal of Emergency Medicine found that adults who reported a first‑ or second‑degree relative with acute appendicitis were about 2‑3 times more likely to develop it themselves.
- An observational study from Jordan (2018) reported an even sharper increase—up to 10‑fold higher risk for people under 30 when a close relative had the condition.
- A recent 2025 Healthline summary noted that genetics might play a role, but that “the cause of appendicitis is often unclear.”
What this all tells us is simple: a positive family history of appendicitis is a red flag worth noting, but it’s far from a death sentence.
Genetic Findings
Scientists have started to dig into the DNA puzzle, and a few clues have emerged.
| Gene / Variant | What It Does | Impact on Risk |
|---|---|---|
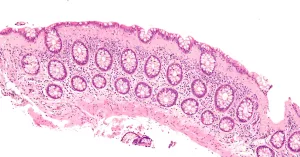
| HLX | Regulates inflammatory response in appendix tissue | Higher expression linked to increased inflammation |
| CTSB | Encodes cathepsin B, an enzyme involved in tissue remodeling | More active in inflamed appendix; may aid blockage formation |
| NEDD4L | Controls sodium and water transport in gut cells | Variations may alter appendix fluid balance, raising susceptibility |
These findings come from a 2022 genetic study highlighted by Healthline and a 2024 JAMA Surgery article that identified the NEDD4L gene as a possible player. The key takeaway? Genetic variations explain only a slice of the puzzle—they’re one piece among many, and they don’t guarantee you’ll get appendicitis.
Lifestyle Triggers
Here’s where the story gets interesting: the same genes that whisper “higher risk” can be silenced—or at least muffled—by everyday choices.
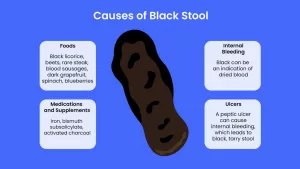
Blockage is the most common immediate cause. Hardened stool, a small growth, or even a viral infection can clog the appendix lumen, leading to swelling and pain. If you’re already genetically predisposed, that blockage can tip the scales.
Research from 2023 shows a clear link between diet and appendicitis risk:
- Low‑fiber diets (think processed snacks, white bread, sugary drinks) increase the likelihood of hard stool formation.
- High sugar intake may promote inflammation and alter gut flora, making blockages more probable.
- Smoking has also been correlated with a modest rise in appendicitis cases, probably because of its impact on immune response.
What does that mean for you? Even if you have a family history, adopting a high‑fiber, water‑rich diet can shrink the risk dramatically. Think of it as giving your appendix a smooth, well‑lubricated runway instead of a bumpy, clogged one.
Testing Options
“Can I get a genetic test and find out if I’m doomed?” you might ask. The short answer: there’s no routine clinical test for appendicitis risk.
Guidelines from major gastroenterology societies advise against screening purely for appendicitis because:
- The predictive value of current genetic markers is still low.
- Testing can be costly and may cause unnecessary anxiety.
- Most importantly, lifestyle modifications remain the most effective preventive tool.
That said, if you belong to a family with multiple early‑onset cases (say, two siblings under 30 who needed surgery), a conversation with a genetics counselor could be worthwhile. They can help you interpret any existing genetic data you might already have (for example, from a broader hereditary‑cancer panel) and give personalized advice.
What To Do If You Have a Positive Family History
Knowing you’re at a slightly higher risk is empowering—not frightening. Here’s a friendly action plan you can start today.
Stay Alert to Early Warning Signs
Appendicitis often begins with a vague, “uh‑oh” feeling in the belly that moves toward the lower right side. Keep an eye out for:
- Sudden, steady pain that starts near the navel and then shifts to the lower right abdomen
- Nausea, loss of appetite, or mild fever
- Changes in bowel habits (constipation or inability to pass gas)
If any of these pop up and last longer than a few hours, give your doctor a call. In the emergency setting, timing matters—most surgeons aim to operate within 24 hours of symptom onset to avoid rupture.
Adopt Proven Preventive Habits
Here’s a quick checklist you can stick on your fridge:
- Fiber up! Aim for at least 25 g of fiber daily—whole‑grain cereals, beans, fruits, and veggies all count.
- Hydrate. Eight cups of water a day keeps stool soft and your gut happy.
- Limit processed sugar. That soda you love? Swap it for water or herbal tea.
- Quit smoking. If you smoke, consider quitting—your whole digestive system will thank you.
- Manage IBD. If you have ulcerative colitis or Crohn’s disease, stay on top of your treatment plan; these conditions are known to increase appendicitis risk.
Talk To Your Doctor
Bring up your family history at your next primary‑care visit. A simple note in your medical record can prompt doctors to be extra vigilant if you ever report abdominal pain. You can even use this short script:
“I have a family history of appendicitis (my mother/sibling had surgery at age X). I’d like to know what signs I should watch for and if any preventive steps are recommended for me.”
Most physicians will appreciate the honesty and will likely suggest a low threshold for imaging (ultrasound or CT) if you develop symptoms.
Wrap‑Up: Knowledge Is Power
To recap:
- Appendicitis is not hereditary in the classic sense, but a family history can boost your risk modestly.
- Genetic studies point to a handful of genes (HLX, CTSB, NEDD4L) that may nudge susceptibility.
- Lifestyle factors—especially diet, hydration, and smoking—play a far larger role and are entirely within your control.
- There’s no routine genetic test, but a conversation with a genetics counselor can be helpful in families with many early‑onset cases.
- Stay alert to early symptoms, keep your gut humming with fiber and water, and let your doctor know about any family history.
Remember, a little extra awareness and a few simple habits can make a massive difference. If you’ve ever watched a loved one scramble to the ER for “appendix pain,” you know how scary it can be. By understanding the mix of genetics and daily choices, you’re giving yourself—and your family—an edge.
What’s your experience with family history and gut health? Have you tried any of the preventive tips above? Drop a comment, share your story, or ask any lingering questions. Let’s keep the conversation going—because when we learn together, we’re all healthier.






















Leave a Reply
You must be logged in to post a comment.