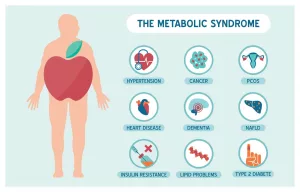
Most people don’t realize that a fatty liver isn’t just a “bad diet” problem. In reality, it’s a metabolic condition that can be managed—or even reversed—by a team of doctors. Whether you’re just starting to hear the term MASLD (the new name for what used to be called NAFLD) or you’ve already been told you have “fatty liver disease,” knowing which doctors treat fatty liver is the first step toward getting your health back on track.
In this friendly, down‑to‑earth guide I’ll walk you through the whole care pathway: from the first chat with your primary‑care doctor to the specialists who dive deeper when the situation calls for it. I’ll sprinkle in real‑world examples, practical checklists, and a few stories from folks who’ve walked this road. By the end you’ll feel confident about who to see, what to ask, and how to make the most of every appointment.
Understanding the Pathway
What Is MASLD?
MASLD (Metabolic Dysfunction‑Associated Steatotic Liver Disease) is the umbrella term for fat accumulation in the liver that isn’t caused by heavy alcohol use. It covers everything from simple steatosis—fat sitting in your liver cells—to the more serious inflammatory stage called NASH (Non‑Alcoholic Steatohepatitis). The good news? It’s incredibly common—about one‑in‑three adults worldwide has some degree of fatty liver—and it’s also reversible when caught early.
The Role of Your Primary‑Care Doctor
Your primary‑care doctor (sometimes called a primary care doctor) is usually the first line of defense. During a routine check‑up they might order liver‑function tests (ALT, AST) and an abdominal ultrasound if anything looks off. If the tests show mild elevation or a “bright liver” on ultrasound, the PCP will probably start the conversation about lifestyle changes—weight loss, coffee, and a bit of exercise—before referring you onward.
When to Step‑Up to a Specialist
If your labs are more than a little abnormal, or if imaging shows fibrosis (scar tissue), it’s time to bring in a specialist. Below is a quick snapshot of who typically steps in and why:
| Condition | Specialist | Why They’re Needed |
|---|---|---|
| Simple steatosis, no fibrosis | Primary‑care doctor | Can monitor, prescribe lifestyle meds, order repeat labs |
| Elevated enzymes + metabolic syndrome | Endocrinologist | Manages insulin resistance, diabetes, thyroid issues that drive liver fat |
| FibroScan ≥ F2 or suspicious imaging | Gastro‑enterologist / Hepatologist | Performs advanced imaging, biopsies, and offers medication options |
| Cirrhosis or high cancer risk | Hepatologist | Handles portal hypertension, transplant evaluation, and advanced therapies |
Key Doctors
Primary‑Care Doctor
Think of your PCP as the friendly neighborhood guide. They’ll order the first blood work, discuss your weight‑loss goals, and set up follow‑up appointments. Many patients feel reassured simply because a familiar face is looking out for them. For example, John discovered his ALT was slightly high during a yearly physical; his doctor suggested a low‑carb diet and a coffee habit (three cups a day) and scheduled a repeat test in three months. The numbers went down, and John never needed a specialist referral.
Gastro‑Enterologist
Gastro‑enterologists are the “gut‑and‑liver” experts. They’ve completed a fellowship that includes intensive training on liver disease, endoscopic procedures, and interpreting FibroScans. When you need a liver biopsy, a prescription for vitamin E, or an evaluation for clinical trial eligibility, they’re the go‑to people. According to the American Association for the Study of Liver Diseases, gastro‑enterologists manage patients with fibrosis stages F2–F3 and initiate first‑line pharmacologic therapy.
Hepatologist
Hepatologists are the ultimate liver specialists—often board‑certified in both gastro‑enterology and hepatology. They dive deep into advanced disease, such as cirrhosis (F4) or liver cancer risk. If you’re facing portal hypertension, variceal screening, or transplant discussions, you’ll likely be in a hepatologist’s care. Their expertise also includes guiding patients through emerging drugs and ensuring you’re linked to appropriate clinical trials.
Endocrinologist
Because fatty liver is tightly linked to insulin resistance, type‑2 diabetes, and hormonal imbalances, an endocrinologist can be a game‑changer. They fine‑tune blood‑sugar control, prescribe GLP‑1 agonists (like semaglutide) that have shown promising reductions in liver fat, and coordinate with your dietitian for a cohesive plan. Maria, a 45‑year‑old teacher, credits her endocrinologist’s “weight‑loss medication plus diet” strategy for a 30 % drop in liver fat measured on MRI.
Other Specialists (When Needed)
- Cardiologist: For patients with high cardiovascular risk, which often runs hand‑in‑hand with fatty liver.
- Nutritionist/Dietitian: To design a realistic, sustainable eating plan (think Mediterranean, not “no‑carb forever”).
- Physical therapist: If joint pain limits exercise, a therapist can help you stay active safely.
Choosing Wisely
Red‑Flag Symptoms
If you notice any of these, book a specialist appointment right away:
- Persistent fatigue or unexplained weakness
- Yellowing of the skin or eyes (jaundice)
- Sudden weight loss or abdominal pain
- Rapid rise in liver enzymes on blood work
Questions to Ask Your Doctor
Having a list of questions shows you’re engaged and helps the doctor focus on what matters most to you. Try asking:
- What stage of fatty liver am I at (F‑score)?
- Do I need a FibroScan or a liver biopsy?
- Which lifestyle changes have the strongest evidence?
- Are there any medication options for my stage?
- How often should I be re‑tested?
Verifying Credentials
Look for board certification in gastro‑enterology or hepatology (in the U.S., the American Board of Internal Medicine). A quick PubMed search of the doctor’s name can reveal whether they’ve published research on MASLD. A reputable source such as the clinicaltrials.gov database can also show if they’re involved in ongoing studies—often a sign of cutting‑edge expertise.
Insurance & Referral Logistics
Many insurance plans require a referral from your primary‑care doctor before you can see a gastro‑enterologist or hepatologist. Call your insurer ahead of time, confirm whether tele‑health visits are covered (they’re great for endocrinology follow‑ups), and keep a copy of any prior imaging or lab reports to speed up the specialist’s review.
Treatment Options
Lifestyle First Prescription
All specialists agree that the cornerstone of fatty liver treatment is weight loss—ideally 7‑10 % of body weight. This can drop liver fat by up to 30 % in many studies. Coffee is a surprising ally; three to four cups a day (without sugar) have been linked to lower liver enzymes. A simple daily routine could look like:
- 30‑minute brisk walk, five days a week
- Swap sugary drinks for water or unsweetened tea
- Include a cup of coffee in the morning
- Focus on whole grains, nuts, and plenty of vegetables
Pharmacologic Options
When lifestyle changes need a boost, doctors may consider off‑label medications. Here’s a quick reference:
| Drug | Indication | Evidence |
|---|---|---|
| Vitamin E (800 IU) | Non‑diabetic NASH | PIVENS trial (NEJM 2010) |
| Pioglitazone | Insulin resistance‑driven NASH | Improves fibrosis in multiple RCTs |
| GLP‑1 agonists (e.g., semaglutide) | Obesity‑related MASLD | Phase‑III trial 2022 showed 30 % liver‑fat reduction |
Remember, none of these drugs are FDA‑approved specifically for fatty liver yet, so your doctor will weigh benefits against potential side effects.
Advanced Interventions
If you have advanced fibrosis or cirrhosis, the hepatologist may discuss:
- Enrolling in a clinical trial—search clinicaltrials.gov for the latest options.
- Regular surveillance for liver cancer (ultrasound every six months).
- Potential liver‑transplant evaluation if liver function deteriorates drastically.
Real Stories
Mike’s Journey – From PCP to Hepatology
Mike, 52, went to his primary‑care doctor for routine blood work and learned his ALT was twice the normal limit. The doctor ordered an ultrasound, which showed a “bright liver” and a FibroScan score of F2. He was referred to a gastro‑enterologist who confirmed moderate fibrosis and started him on vitamin E while enrolling him in a weight‑loss program. Six months later, his FibroScan improved to F1 and his liver enzymes normalized. Mike’s story illustrates how early referral can halt progression.
Aisha’s Turnaround – Endocrinology‑Led Reversal
Aisha, 34, struggled with pre‑diabetes and a diagnosis of MASLD. After a chat with her endocrinologist, she began a GLP‑1 agonist (semaglutide) alongside a Mediterranean‑style diet. Within a year, MRI showed a 25 % reduction in liver fat, and her HbA1c dropped from 6.2 % to 5.4 %. Her experience underscores the power of a metabolic specialist when insulin resistance fuels the liver fat.
Tom’s Ongoing Surveillance – Gastroenterology Care
Tom, 68, was diagnosed with early cirrhosis (F4) after a routine ultrasound during a colonoscopy prep. His hepatologist set up a six‑month ultrasound schedule and prescribed a low‑sodium diet. Although Tom’s liver cannot fully regenerate, careful monitoring has kept complications at bay, and he remains active with daily walks. Tom’s case shows why a liver‑doctor’s expertise is crucial when fibrosis is advanced.
Bottom Line
When it comes to “doctors for fatty liver,” there isn’t a one‑size‑fits‑all answer. Your primary‑care doctor is the friendly first stop, ready to order tests and kick‑start lifestyle changes. If the situation deepens, an endocrinologist can untangle the metabolic knots, a gastro‑enterologist or hepatologist can address fibrosis and medication, and a liver specialist will guide you through advanced surveillance or transplant options.
Take the next step today: schedule that blood test, jot down the questions above, and keep a notebook of your symptoms, meals, and activity. Knowledge is empowerment, and the right doctor‑team can turn a scary diagnosis into a manageable, even reversible, health journey.
What’s your experience with fatty liver care? Have you found a doctor who made a difference? Share your story in the comments below or reach out if you need help finding a specialist near you. We’re all in this together, and every step forward counts.





















Leave a Reply
You must be logged in to post a comment.