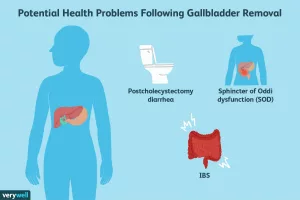
If you’ve ever wondered why your stomach sometimes feels like a tight knot on the left side and other times like a dull ache across the whole belly, you’re not alone. Most people with irritable bowel syndrome (IBS) notice that the pain can jump around, and that can feel both confusing and frustrating.
Here’s the quick answer: the typical spot is the lower abdomen, especially the left side, but the pain can move to the middle, right side, or even up toward the ribs depending on what you ate, how stressed you are, and which IBS subtype you have. Knowing where the pain shows up helps you predict what might make it better (or worse) and gives your doctor a clearer picture when you finally sit down for that appointment.
Why Pain Moves
Gut Anatomy Basics
Think of your intestines as a long, winding highway. The descending colon runs down the left side of your belly, the sigmoid curves into the pelvis, and the ascending colon climbs up the right side. When the muscle walls of these sections spasm or become overly sensitive, the pain follows the road – usually showing up where the colon is most active.
IBS Sub‑types Influence
IBS isn’t a one‑size‑fits‑all condition. It splits into three main sub‑types, and each has its own “pain map.”
- IBS‑C (constipation‑predominant) – you’ll often feel cramping in the lower left quadrant because the stool lingers in the descending colon.
- IBS‑D (diarrhea‑predominant) – sharp, urgent pain tends to pop up on the lower right side where the ascending colon pushes waste forward quickly.
- IBS‑M (mixed) – a blend of both, so the pain can flip‑flop between left, right, or even sit in the middle.
Triggers That Shift Pain
Even within the same day, different triggers can pull the pain to new neighborhoods. Here are the usual suspects:
| Trigger | Typical Spot | Typical Sensation |
|---|---|---|
| Large, high‑fat meal | Lower left | Cramping, gas‑filled pressure |
| Stress or anxiety | Mid‑abdomen | Tight, “muscle‑like” ache |
| Sudden diarrhea episode | Lower right | Sharp, urgent stabbing |
| Hormonal shift (e.g., menstrual cycle) | Across lower abdomen | Diffuse bloating‑related pain |
Notice the pattern? When we eat a big meal, the gut stretches, and the left side—where the descending colon hangs out—often feels the most pressure. When we’re stressed, the whole gut can go into overdrive, giving a central, tighter feeling. Knowing these patterns can feel like having a personal weather map for your belly.
In fact, according to Healthline, many people experience a shifting pain pattern that doesn’t point to something more serious, but it does highlight how sensitive the gut can be to everyday triggers.
Describing Sensations
Cramp vs Sharp vs Ache
Words matter. If you describe your pain as “cramping,” you’re hinting at rhythmic muscle contractions—typical of IBS. “Sharp” or “stabbing” often signals a sudden, high‑intensity contraction, more common with IBS‑D. “Aching” or “dull throbbing” usually lasts longer and is seen in IBS‑C when stool sits too long.
Day‑to‑Day Variation
It’s not unusual to wake up with a mild, lingering ache, feel a spike of sharp pain after lunch, and then notice a gentle cramp after an evening walk. Researchers call this “visceral hypersensitivity” – the gut’s nerves become extra‑responsive, turning everyday sensations into pain signals.
Mini‑Case: Anna, 34, IBS‑C
Anna kept a pain diary for two weeks. On Monday morning she felt a low‑grade ache in the lower left quadrant after a coffee‑heavy breakfast. By lunchtime, a big bowl of pasta sent a wave of cramping through the same spot, easing only after a slow, steady bowel movement. Wednesday evening, a stressful meeting gave her a sudden tightness in the mid‑abdomen that lasted 30 minutes before fading. By the end of the week, she realized that coffee, large meals, and stress each had a distinct “pain fingerprint.”
Anna’s story illustrates why the exact location and quality of pain matter—they’re clues you can use to outsmart IBS.
When to Seek Help
Red‑Flag Symptoms
IBS pain is uncomfortable, but it’s rarely a sign of a life‑threatening problem. However, if any of the following appear, it’s time to call a healthcare professional:
- Fever or chills
- Blood in stool or black, tar‑like stools
- Unexplained weight loss
- Pain that worsens sharply with movement or does not improve after a bowel movement
- Persistent vomiting or inability to keep food down
What Doctors Look For
When you finally meet with a gastroenterologist, they’ll ask you to draw a “pain map” on a simple template. This visual lets them see patterns you might miss when you just describe sensations verbally. The doctor will also compare your diary against the Rome IV criteria—three essential elements: recurrent abdominal pain at least one day per week in the past three months, plus two of the following (pain related to defecation, change in stool form, or change in stool frequency).
Downloadable Pain‑Tracking Sheet
Below is a quick‑fill template you can print (or copy into a notes app). Fill in the time, food, stress level, and where the pain was felt. Over a week you’ll have a story to show your doctor.
Date | Time | Food/Drink | Stress (1‑10) | Pain Location | Sensation | Duration | Relief?---------------------------------------------------------------------------
Having this record not only speeds up diagnosis, it also empowers you to notice which triggers you can tame.
Managing By Location
Targeted Food Tweaks
Not all “IBS diets” are created equal. If you notice that lower‑left cramping flares after high‑FODMAP foods (like onions, garlic, or wheat), a low‑FODMAP trial can quiet that spot. Conversely, if right‑side stabbing appears after dairy, a trial of lactose‑free products may help.
Stress‑Relief Tools
Because stress fuels visceral hypersensitivity, calming the mind can calm the gut. Try any of these, even for just five minutes a day:
- Deep belly breathing: inhale for four counts, hold for four, exhale for six.
- Guided mindfulness apps (many have free versions).
- Gentle yoga poses—Child’s Pose and Supine Twist are especially gut‑friendly.
Medication & Probiotics
When lifestyle tweaks aren’t enough, physicians may prescribe:
- Antispasmodics (e.g., hyoscine butylbromide) to relax the intestinal muscle.
- Rifaximin for IBS‑D, especially when bloating is a major issue.
- Specific probiotic strains like Bifidobacterium infantis that have shown modest benefit in reducing abdominal pain.
Always discuss any supplement with your doctor first; what works for one person’s left‑side cramps may not help another’s right‑side spikes.
Real Experiences
Patient Stories
“I used to think my pain was just ‘stomach upset.’ After keeping a pain diary, I realized the cramp in my lower left abdomen always came after a big coffee, while the sharp jab on the right side showed up after an anxious meeting. Adjusting my caffeine and practicing quick breathing reduced both by half,” says Mark, 42.
“My IBS‑C made me dread any meal because the ache would linger for days. When I started a low‑FODMAP plan focused on the left side, the dull ache faded, and I could finally enjoy brunch again,” shares Lina, 29.
Expert Insight
Dr. Christos Zavos, a gastroenterologist based in Thessaloniki, notes: “The location of pain is a valuable diagnostic clue. If a patient reports constant left‑lower‑quadrant discomfort, we think about constipation‑related IBS first, but we also rule out other causes like diverticulitis. A clear pain map speeds up that process.”
Nutritionist Emily Cole, RDN, adds: “Food isn’t the only trigger; the gut–brain connection means emotional states shift pain patterns. Helping patients track both what they eat and how they feel creates a powerful feedback loop for self‑management.”
Putting It All Together
Understanding IBS pain location isn’t just academic—it’s a practical roadmap that can guide you toward relief. The lower abdomen, especially the left side, is the most common hotspot, but the pain can wander to the right, the middle, or even up toward the ribs depending on meals, stress, and your IBS subtype.
By learning the anatomy, noting the quality of each sensation, and keeping a simple pain diary, you give yourself—and your doctor—the tools to pinpoint triggers and choose smarter treatments. Whether it’s a targeted low‑FODMAP tweak, a quick breathing break, or a prescription antispasmodic, the right approach often starts with the simple question: Where does it hurt?
So grab a pen, sketch that pain map, and let’s start turning those mysterious belly signals into clear, actionable insights. Your gut will thank you, and you’ll feel a little more in control of each day.
What’s your biggest challenge with IBS pain? Share your story in the comments, or reach out if you have questions—let’s navigate this together!



















Leave a Reply
You must be logged in to post a comment.