Why Everyone’s Suddenly Talking About Breast Density
Imagine sitting in a waiting room, phone in hand, scrolling through cat videos—nervous energy buzzing. The nurse calls your name, and, after a few polite questions, hands you a report from your latest mammogram. “Dense breasts,” it reads. That’s it. Wait…what? Am I supposed to panic? Call my mom? Or just shrug and get a fancy coffee?
If this scene feels familiar, you are so not alone. Here’s a wild stat: nearly half of women over 40 get the “dense breasts” headline after a routine screening (dense breast tissue: what it means). And yet, most of us are left to Google—and spiral—alone. Let’s fix that.
So…What Does “Dense” Even Mean?
Is This Normal? Why Me?
Don’t worry—having dense breasts isn’t rare, dangerous, or even that weird. It just means your boobs have more “busy” tissue (gland and fibrous stuff) compared to fatty tissue. It’s like how some lattes are milkier and some are extra foamy; it’s all coffee, just different recipes.
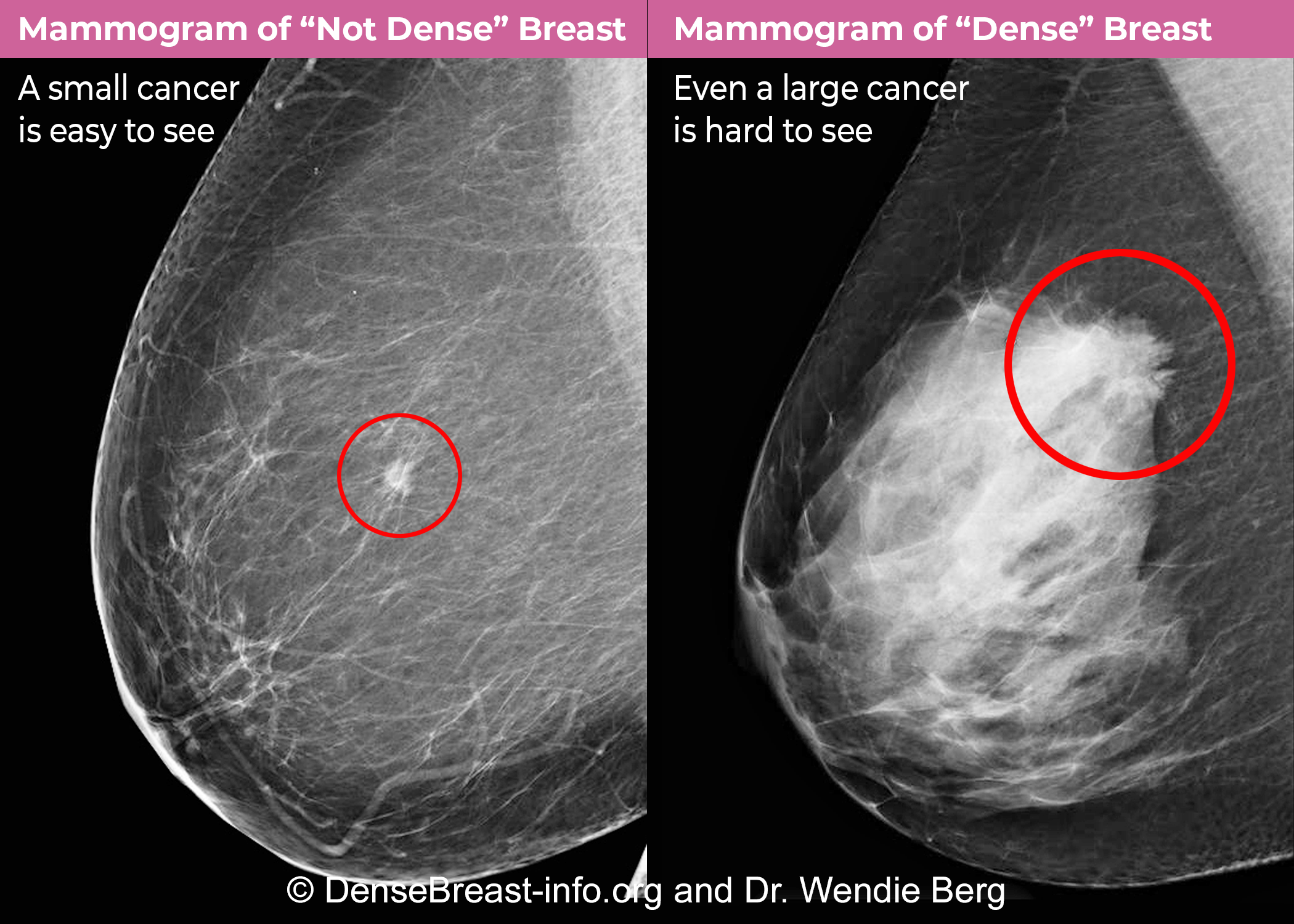
A dense reading isn’t a diagnosis. It doesn’t mean cancer. Here’s where it does matter: Dense tissue looks white on a mammogram, and guess what else does? Tumors. So sometimes things can hide…sneaky, right? That’s why extra follow-up is a thing. But relax—most people with dense breasts never develop anything scary.
Let’s Get Visual: Understanding Your Results
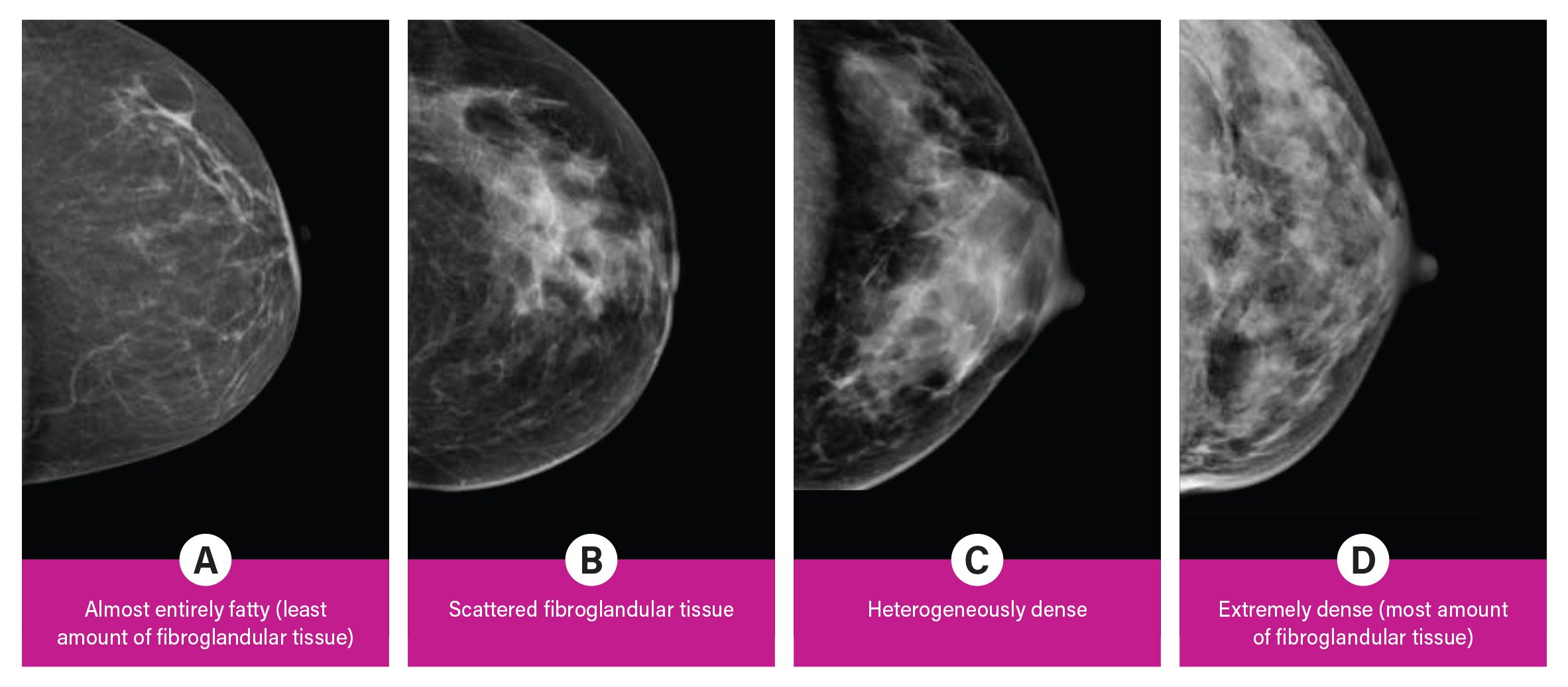
Okay, picture your mammogram like a blackboard. Fatty tissue is see-through chalk; dense tissue is like dried glue—hard for the radiologist to peek through. Radiologists use something called BI-RADS levels (think grades from A to D) to describe density:
| BI-RADS Level | What It Looks Like | Cancer Spotting Ease |
|---|---|---|
| A (Fatty) | Mostly fat | Super clear |
| B (Scattered) | Some dense spots | Pretty good |
| C (Heterogeneous) | Patchy dense areas | Trickier |
| D (Extreme) | Almost all dense | Hardest to see |
My friend Alex once joked her scan looked like a snowstorm—not ideal unless you’re planning a ski trip. But her doc explained: “It just means we’ll keep an extra eye out. No need to freak.” Good to know, right?
Cracking The Dense Breast ICD-10 Code
Wait, ICD-What? Why Does This Code Matter?
Okay, hang with me—promise this is simpler than it sounds (and not just “doctor talk”). ICD-10 codes are these short numbers and letters hospitals use to label and track health findings. Think of them as quick notes so your health info goes where it needs to—insurance, specialists, you name it.
For dense breasts, the code you’ll bump into most is R92.30, which means “dense breasts, unspecified.” It’s kind of the default—like the “medium” setting on a blender. If your radiologist doesn’t get super specific about the BI-RADS level, they use this one (dense breast icd 10).
But the ICD-10 world gets way more granular if needed (nobody said healthcare was simple):
Here’s How They Break Down:
| Code | Description | When It’s Used | Hot Tip |
|---|---|---|---|
| R92.30 | Dense breasts, unspecified | Initial, not super-detailed finding | Most common code for insurance |
| R92.31 | Fatty replaced breasts (BI-RADS A) | Your tissue is mostly fat | Rare for dense reports |
| R92.32 | Scattered fibroglandular density (BI-RADS B) | Some dense spots, mostly clear | Lower risk for hiding things |
| R92.33 | Heterogeneously dense (BI-RADS C) | Patchy dense tissue, can hide stuff | Ask for details if you get this |
| R92.34 | Extremely dense (BI-RADS D) | Almost all dense, very hard to scan | You may need extra tests |
I remember helping my cousin Sam decode her own R92.30 “mystery.” All it meant: she needed to come back for a different type of scan next year. She panicked at first…but ended up relieved once it was laid out like this.
Want the deep dive? There’s a whole world of practical tips in this dense breast icd 10 guide, too.
Could Dense Breasts Cancel My Cancer Screening?
Hang On…Am I At Risk Now?
This is the question, isn’t it? Here’s the bottom line: having dense breasts doesn’t mean you have cancer, or will get it. What it does is make certain cancers sneakier—hiding in plain sight behind all the “white” on your x-rays. Ugh, right?
Your risk creeps up a bit—people with the densest tissue have four times the risk compared to those with mostly fatty breasts according to research on dense breast tissue. But even so, most cancers are still caught with regular screening. The trick is…sometimes, you’ll need extra tests. That’s where these ICD-10 codes really earn their keep. They flag your file so insurance and your docs know to boost vigilance. And that’s a good thing.
What Happens Next? Extra Scans, Maybe…
Getting a dense breast flag may mean more than just an annual mammogram—especially if you’re at high risk (hello, strong family history). Options could include 3D tomosynthesis (a sort of “slices” x-ray—way cooler clarity) or breast MRI, which can pick out cancers even in the thickest tissue (insurance billing codes).
Real-life shoutout: A reader messaged me last year, saying her R92.33 code helped her and her doctor push for an MRI that actually found a stage 1 tumor—super early, totally removable. So that little ICD-10 box? Sometimes, it’s life-changing.
| Screening Option | When to Consider | What to Expect |
|---|---|---|
| 3D Mammogram | If regular scans look hazy | Better layering, clearer results |
| MRI | Family history or very dense breasts | No radiation, super sensitive |
| Ultrasound | Quick check after something odd | Hand-held, easy, sometimes insurance covers it |
Yes, insurance and codes can be a pain…but having the right code (dense breast icd 10) can really open doors.
Let’s Talk About Your Next Steps
Do I Just Wait For The Next Mammogram?
Not necessarily. If you get a dense breast finding, open a direct line to your provider. Ask: What’s my BI-RADS category? Am I in the “hard to read” zone? Should I have any extras this year? And—can you make sure my record is coded as R92.30 (or whichever matches best), so nothing falls through the cracks?
There’s actually comfort in getting technical sometimes. It keeps everyone—doctors, insurance, and you—on the same page. And it means next year’s scan, or the one after, won’t be a mad scramble for answers.
My Favorite Takeaway? You’re In Charge.
You can always ask for your mammogram report and read it yourself (or bring it to a friend who understands these codes—trust me, we exist). Gently push for dense breast icd 10 accuracy, insist on more details about your breast density, and discuss any extra test recommendations.
And if you’re thinking “But I’m healthy! Do I really need this?”—just remember, early info is power, not a punishment.
Let’s Wrap This Up: Action, Not Anxiety
If you zoned out somewhere around “ICD-10,” come back for a second—it’s worth it! Here’s what actually matters: Dense breasts are super common, not scary, but they do mean you’ll want to stay a little more plugged in about your screening. Knowing those codes—like R92.30, R92.33, and the rest—can turn a mystery into a plan. They make a difference, especially if you ever want a second opinion or need to nudge insurance for advanced imaging.
Get your BI-RADS level in your records. Push for accurate, specific notes (don’t let “unspecified” be your default if you can avoid it!). And if you’re over 40, have family risk, or just want peace of mind, chat with your provider. Seriously—bring a list of questions, and don’t leave until you understand your situation. The dense breast icd 10 world is only confusing until it isn’t.
And finally—don’t let the dense breast talk scare you into silence. Early action (even one awkward phone call or a weirdly specific code written down) can be a massive win for your long-term health. So…read your report, share this info with a friend, ask all the “dumb” questions you want (they’re not), and keep showing up for yourself. That’s what health is about. Pinky promise.























Leave a Reply
You must be logged in to post a comment.