Hey there, friend. If you’ve just gotten a blood test that says “low hemoglobin” and you’re living with HIV, you might be wondering what that really means. Is it a sign that your virus is getting worse? Should you be worried about your energy levels? The short answer is: you’ve probably encountered HIV‑related anemia, a fairly common companion on the HIV journey. In the next few minutes we’ll break down exactly why it happens, how you can spot it early, and what you can do to feel better again. No fluff, just straight‑to‑the‑point help you can use right now.
What Is HIV‑Related Anemia
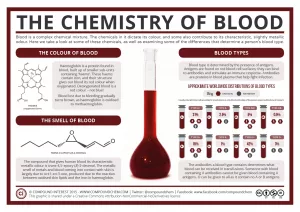
In plain language, anemia is when you don’t have enough healthy red blood cells (RBCs) or hemoglobin to carry oxygen around your body. When you add HIV into the mix, the picture gets a bit more complicated. Studies show that anywhere from 7 % to 50 % of people on antiretroviral therapy (ART) develop anemia, and the risk shoots up when your CD4 count falls below 200 cells/µL (Johns Hopkins).
Why is it different from “regular” anemia? HIV can directly suppress the bone marrow—where blood cells are made—through inflammatory cytokines, it can blunt the body’s natural response to erythropoietin (the hormone that tells the marrow to crank out more RBCs), and many of the medicines we take to keep the virus in check have anemia as a side effect. In short, the virus, the treatment, and your body’s own reaction all team up to lower your hemoglobin.
Quick FAQ
- Is HIV‑related anemia the same as iron‑deficiency anemia? Not usually. Iron deficiency is just one possible cause; HIV‑related anemia often stems from marrow suppression or chronic inflammation.
- What hemoglobin level counts as anemia? For men, < 13 g/dL; for women, < 12 g/dL. Values under 10 g/dL usually start to cause noticeable symptoms.
Key Numbers at a Glance
| Population | Prevalence of Anemia | Typical Hgb Range (g/dL) |
|---|---|---|
| General HIV‑positive (ART era) | 7–50 % | 9–12 |
| CD4 < 200 cells/µL | ~30 % | 8–10 |
| On zidovudine (AZT) | 15–20 % | 7–9 |
Spotting Anemia Symptoms
Feeling a little more tired than usual? That could be the first whisper of anemia. The classic symptoms—fatigue, shortness of breath on modest exertion, a racing heartbeat, and a pale complexion—often appear when hemoglobin dips below 10‑11 g/dL (Johns Hopkins). As the numbers fall further (under 8‑9 g/dL), you might notice dizziness, chest discomfort, or even confusion.
Besides the “feel‑the‑fatigue” warning lights, a simple CBC (complete blood count) can tell the whole story. Look for:
- Low hemoglobin (Hgb)
- Low hematocrit (Hct)
- Mean corpuscular volume (MCV) that’s usually normal (normocytic) in HIV‑related anemia
- Reticulocyte count—if it’s low, your marrow isn’t making enough new cells.
When to Call Your Doctor
If you experience any of the following, pick up the phone:
- Rapid heart rate > 100 bpm at rest
- Shortness of breath while walking a short block
- Chest pain or pressure
- New confusion or difficulty concentrating
Lab‑Interpretation Flow
Low reticulocyte + low iron → think iron deficiency; low reticulocyte + normal iron → suspect marrow suppression; high LDH + high bilirubin → hemolysis. This quick cheat‑sheet helps you talk intelligently with your clinician about what’s really going on.
Why Anemia Happens
Let’s unpack the main culprits one by one. Knowing the “why” makes it easier to target the right fix.
Direct HIV Effect on Bone Marrow
HIV can infect marrow stromal cells and release cytokines that shut down erythropoietin production (JID review). The result? Fewer red cells are born, even if iron and vitamins are plentiful.
Nutritional Deficiencies
Malabsorption, chronic diarrhea, and some ART drugs steal vitamins right out from under you. B12, folate, and iron deficits are common, especially if you’re dealing with opportunistic infections that affect the gut.
Medication‑Induced Anemia
Older NRTIs like zidovudine (AZT) are notorious for causing macrocytic anemia. Other agents—dapsone, sulfamethoxazole‑trimethoprim (Septra), and even interferon—can also knock your red cell count down (The Body).
Opportunistic Infections & Malignancies
Things like Mycobacterium avium complex, tuberculosis, or lymphoma can infiltrate the marrow or trigger severe inflammation, both of which reduce RBC output.
Chronic Inflammation & “Inflamm‑Aging”
Even when the virus is suppressed, HIV leaves a lingering inflammatory footprint that can sabotage blood production. A 2024 study in Viruses highlighted how chronic anemia can strain the heart and kidneys in people with HIV (Viruses 2024).
Rare Causes
Sometimes you run into unusual suspects—thrombotic microangiopathy, hemophagocytic lymphohistiocytosis, or even parvovirus B19 infection. While uncommon, they’re worth keeping on the back‑of‑your‑mind if routine work‑up comes up empty.
Cause‑by‑Prevalence Table
| Cause | Typical CD4 Range | How Common |
|---|---|---|
| Marrow suppression by HIV | Any | High |
| Drug toxicity (AZT, dapsone) | Any | Moderate |
| Nutrient deficiency | Low–moderate | Moderate |
| Opportunistic infection | <200 | Variable |
| Malignancy (lymphoma) | <200 | Low‑moderate |
Treatment Options Overview
Great news: most cases of HIV‑related anemia can be corrected once we know the underlying cause. Think of treatment as a layered cake—start with the easiest, cheapest layer, then add more specialized toppings if needed.
Fix the Root Cause First
Give your body what it’s missing. If labs show low B12, start a monthly injection; if iron is low, add a gentle oral supplement. Treat any active opportunistic infection (e.g., MAC) and consider switching out a marrow‑toxic ART drug for a newer integrase inhibitor.
Erythropoiesis‑Stimulating Agents (ESA)
When anemia persists despite fixing the basics, drugs like epoetin alfa or darbepoetin can jump‑start red‑cell production. The 2004 expert panel in Clinical Infectious Diseases recommended ESA for hemoglobin < 10 g/dL when other measures have failed (CID 2004).
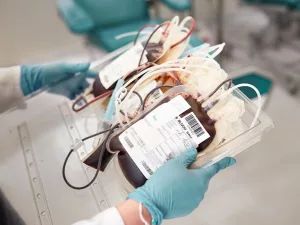
Blood Transfusion
In emergencies—say your Hgb drops below 7 g/dL or you develop chest pain—transfusion is the fastest way to restore oxygen delivery. It’s a temporary bridge while you sort out the long‑term plan.
Adjunct & Experimental Therapies
Research is exploring IL‑6 blockers and other anti‑inflammatory agents to curb the chronic inflammation that fuels anemia. These are still mostly in trial phases, but they signal a future where we can target the “inflamm‑aging” pathway directly.
Lifestyle & Supportive Care
Don’t underestimate the power of good sleep, regular low‑impact exercise, and staying hydrated. Even modest activity (like a daily 20‑minute walk) can improve circulation and boost energy levels.
Treatment Decision Tree
1️⃣ Identify cause → 2️⃣ Correct nutritional/drug issues → 3️⃣ Consider ESA if Hgb < 10 g/dL → 4️⃣ Transfusion for acute severe drops → 5️⃣ Follow‑up labs every 4‑6 weeks.
Living With Anemia
Now, let’s talk about the day‑to‑day. How do you keep living a full life while juggling HIV and anemia?
Real‑World Stories
Mike, 38, on AZT – After months of feeling “zombie‑like,” a simple B12 shot lifted his hemoglobin from 9.2 to 11.8 g/dL and his energy back to “I could run a marathon” (well, metaphorically). He switched his regimen to an integrase‑based combo and hasn’t looked back.
Lena, 52, CD4 150 – Her anemia persisted despite supplements. The doctor switched her from zidovudine to dolutegravir, added a low‑dose ESA, and within six weeks her Hgb rose to 12.3 g/dL. She now reports feeling “like herself again” and can keep up with her grandkids.
Self‑Monitoring Checklist
- Record daily energy level (1‑10 scale)
- Note any new shortness of breath or palpitations
- Track hemoglobin results after each treatment change
- Ask your clinician about medication side‑effects at every visit
Questions to Ask Your Provider
- What is likely causing my low hemoglobin?
- Should I change any of my HIV meds?
- Do I need iron, B12, folate, or an ESA?
- How often should I repeat labs?
- What warning signs mean I need urgent care?
Printable “Anemia Action Sheet”
Consider creating a one‑page handout with the checklist above, your latest lab values, and your next appointment date. Having it on the fridge can turn a vague worry into a concrete plan.
Bottom Line Summary
HIV‑related anemia may feel like an extra weight on an already heavy load, but it’s also a sign that there’s a clear target for treatment. By catching symptoms early, understanding the tangled web of causes, and working with your care team on a step‑wise plan—nutrient fixes, medication tweaks, ESA therapy, or transfusion when needed—you can reclaim the energy and confidence that anemia steals.
Remember, you’re not alone in this. Your clinicians, community, and even the research literature are all on your side, ready to help you fine‑tune your health. Keep an eye on your labs, speak up about every new symptom, and never hesitate to ask “What can we try next?” The journey to feeling better is a partnership, and you’ve already taken the first, most important step: seeking the information you need.





















Leave a Reply
You must be logged in to post a comment.