Quick answer: A congenital heart defect (CHD) is a structural problem of the heart that’s present at birth. Roughly 1 % of newborns – about 40 000 babies each year in the United States – are born with some form of CHD.
Why it matters: Even a “small” defect can cause low oxygen, feeding trouble, or later‑life complications such as pulmonary hypertension or arrhythmias. This guide shows you how to spot the signs, understand the most common defect types, and navigate today’s treatment options – from pediatric heart valve repair to replacement heart valve surgery.
What Is a CHD?
When doctors say “congenital,” they simply mean “present at birth.” A CHD occurs when the heart or the great vessels around it don’t develop the way they should during the first weeks of pregnancy. The result can be anything from a tiny “hole” between chambers to a missing valve or even an entirely absent chamber.
Unlike adult heart disease, which usually stems from wear‑and‑tear or lifestyle factors, CHDs are structural from day one. According to the CDC, they are the most common birth defect in the United States.
What does “congenital” really mean?
It’s a fancy word for “born with it.” The defect is baked into the heart’s blueprint before the baby takes its first breath.
How do CHDs differ from adult heart disease?
| Aspect | Congenital Heart Defect | Adult Heart Disease |
|---|---|---|
| Origin | Developmental error in utero | Acquired later in life (e.g., atherosclerosis) |
| Typical age of detection | Prenatal or early childhood | Adulthood, often after symptoms appear |
| Treatment focus | Repair or restructure anatomy | Manage flow, remove blockages, lifestyle changes |
What are the main categories of CHDs?
- Septal defects – holes between chambers (ASD, VSD).
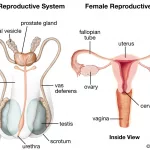
- Valve abnormalities – stenosis or regurgitation of aortic, pulmonary, mitral or tricuspid valves.
- Complex cyanotic defects – Tetralogy of Fallot, hypoplastic left heart syndrome (HLHS), transposition of the great arteries.
- Mixed or rare forms – single‑ventricle physiology, truncus arteriosus.
How Common Are CHDs?
Every year, about 40 000 babies in the U.S. are diagnosed with a CHD – that’s roughly one out of every 100 live births. The numbers haven’t changed dramatically, but survival rates have skyrocketed thanks to better screening and treatment.
Who’s at higher risk?
Most CHDs appear without a clear cause, but certain factors increase the odds:
- Genetic predisposition – inherited mutations or chromosomal abnormalities.
- Maternal health – pre‑existing diabetes, obesity, or lupus.
- In‑utero exposures – certain prescription drugs, alcohol, smoking, or rubella infection.
- Family history – a sibling or parent with a CHD raises the chance.
Does family history matter?
Yes. If a close relative has a CHD, a genetics counselor can discuss testing options and help you understand the likelihood for future pregnancies.
Signs & Symptoms
Every heart is different, so symptoms can vary widely. However, there are some red‑flag clues that parents, caregivers, and even teachers should know.
Newborn red flags
- Persistent cyanosis – a bluish tint to the skin, lips, or nails.
- Rapid or labored breathing.
- Difficulty feeding or poor weight gain.
- Unexplained low blood pressure.
- Heart murmur heard on routine exam.
Symptoms in toddlers and older children
- Shortness of breath with mild activity.
- Chest pain or tightness during exertion.
- Frequent fainting (syncope).
- Reduced growth despite adequate nutrition.
- Exercise intolerance – tiring quickly during play.
Adult‑onset issues from untreated CHD
Even if a defect seemed “minor,” it can set the stage for later problems such as pulmonary hypertension, arrhythmias, infective endocarditis, or heart failure. Regular check‑ups keep these risks in check.
Common Types
Septal Defects (ASD & VSD)
These are “holes” between the heart’s chambers. An atrial septal defect (ASD) connects the two atria, while a ventricular septal defect (VSD) links the ventricles. Small VSDs often close on their own; larger ones may need a patch or a catheter‑based device closure.
Valve‑Related Defects
When a valve is too narrow (stenosis) or leaky (regurgitation), blood can’t flow smoothly. Common examples include aortic valve stenosis and pulmonary valve stenosis. Modern pediatric heart valve repair techniques often avoid the need for a full replacement.
Valve‑repair versus valve‑replacement
| Factor | Repair | Replacement |
|---|---|---|
| Invasiveness | Less invasive, often catheter‑based | Open‑heart surgery (more invasive) |
| Durability | Depends on defect; may need future interventions | Mechanical valves last decades; tissue valves last 10‑15 years |
| Anticoagulation | Usually none | Mechanical valves require lifelong blood thinners |
Complex Cyanotic Defects
These include Tetralogy of Fallot, hypoplastic left heart syndrome (HLHS), and transposition of the great arteries. They often need staged child cardiac surgery and lifelong cardiology follow‑up.
How Are CHDs Diagnosed?
Prenatal screening
Between weeks 18‑24, a fetal echocardiogram can visualize the baby’s heart. If a defect is suspected, the delivery team can prepare for immediate care. Pulse‑oximetry screening within the first 24‑48 hours after birth also helps catch critical CHDs before the baby leaves the hospital.
Post‑natal tests
- Physical exam – listening for murmurs.
- Electrocardiogram (ECG) – checks rhythm.
- Echocardiography – the workhorse imaging tool.
- Cardiac MRI or CT – detailed anatomy for complex cases.
- Genetic testing – recommended when multiple anomalies appear.
When to seek specialist care
If any red flag appears, schedule an appointment with a pediatric cardiology team. They can order the appropriate imaging and, if needed, refer you to a surgeon for replacement heart valve or other interventions.
Treatment Options
Treatment isn’t one‑size‑fits‑all. It depends on defect type, severity, the child’s size, and overall health.
Medication‑only approaches
Some mild defects require only drugs to manage symptoms – prostaglandins to keep ductus arteriosus open, diuretics to reduce fluid overload, or beta‑blockers to control heart rate.
Catheter‑based interventions
These minimally invasive procedures can close holes or widen narrowed vessels using balloons or tiny devices. Success rates for VSD closure, for example, exceed 95 % in experienced centers.
Surgical repair
When anatomy needs reshaping, surgeons perform open‑heart repairs. Common procedures include patching a VSD, reconstructing a malformed valve, or establishing new pathways for blood flow in complex defects.
Valve repair and replacement
For valve problems, surgeons first attempt repair because it preserves the patient’s own tissue and avoids lifelong anticoagulation. If repair isn’t feasible, a replacement heart valve – either mechanical or tissue – is implanted. Children often receive a tissue valve that can grow with them, followed by a later replacement.
Multi‑stage “child cardiac surgery”
Complex single‑ventricle physiologies, such as HLHS, require a series of operations (e.g., Norwood, Glenn, and Fontan procedures). Each stage stabilizes the circulation while the child grows, ultimately allowing the heart to function with one effective ventricle.
Post‑operative care & lifelong follow‑up
Even after a successful repair, regular cardiology visits are essential. Imaging, exercise testing, and sometimes heart valve testing keep the team aware of any subtle changes that might need attention.
Living With CHD
For many families, the journey continues long after the surgeon’s sutures are removed. Here’s what day‑to‑day life often looks like, and how you can thrive.
Routine follow‑up
Most children see their cardiologist every 6‑12 months. The schedule may become less frequent in adulthood, but lifelong monitoring is still recommended, especially for those with repaired valve disease.
Activity and sports
Most kids with repaired CHDs can join regular school sports, but a cardiology clearance is important. Low‑impact activities (swimming, cycling) are usually safe; high‑intensity sports may need individualized assessment.
Pregnancy considerations
Women with CHDs should discuss family planning with their cardiologist early. Some defects increase the risk of complications during pregnancy, but careful monitoring and medication adjustments can lead to healthy outcomes.
Psychosocial support
Living with a chronic condition can be stressful. Support groups, counseling, and school‑based accommodations help children maintain confidence and academic performance. The “Heart Heroes” programs offered by the CDC and AHA provide community and resources.
Transition to adult care
Around ages 16‑21, patients should move from pediatric to adult congenital heart disease (ACHD) specialists. A smooth transition ensures continuity of care and reduces the chance of missed appointments.
Key Take‑aways
Congenital heart defects are common, but thanks to modern medicine, most children grow up to lead full, active lives. Early detection, accurate diagnosis, and personalized treatment—whether a simple medication, a catheter‑based repair, or a staged child cardiac surgery—make all the difference. If you notice any warning signs, don’t wait: talk to a pediatric cardiology specialist, explore heart valve testing if needed, and stay proactive about follow‑up care.
Remember, you’re not alone on this journey. Physicians, nurses, counselors, and countless families have walked this path and are eager to share their knowledge. Stay curious, ask questions, and trust that with the right team, a congenital heart defect is a challenge you can manage—often with a smile as bright as the one on the brave little patients who inspire us every day.




















Leave a Reply
You must be logged in to post a comment.