
So, How Long Really?
Let’s skip the medical jargon and cut to the chase. What does open heart surgery recovery time really look like? What can you expect—not just in theory, but in day-to-day, real, messy life? If you’re prepping for surgery (or helping someone who is), you probably want the truth, not just a list of restrictions and milestones. I’ve watched my uncle, my best friend’s mom, and even my grumpy ex-boss go through it… and trust me, it’s a rollercoaster, but knowing the ride helps.
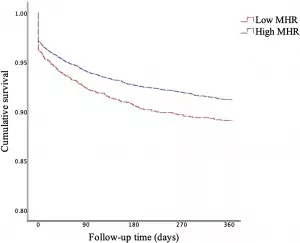
The answer no one really loves: open heart surgery recovery time depends. For most people, we’re talking 6 to 12 weeks before you feel like yourself again, but there are layers to this story. Sometimes you’ll notice big leaps (“Wow, I can walk to the mailbox!”), sometimes it’s two steps forward, one step back. And not to scare you, but boredom and frustration are part of the healing, too.
Why It’s Not a Straight Line
What Makes Recovery Longer (Or Quicker)?
Ever wonder why your neighbor bounced back in four weeks, but your cousin needed three months? It’s not magic. It’s about a few key things:
- What shape you were in before surgery. (Were you walking every day or couch-bound?)
- Your age. (Younger folks often recover quicker. Curious? Dig into Open heart surgery survival rate by age—some real surprises in those stats.)
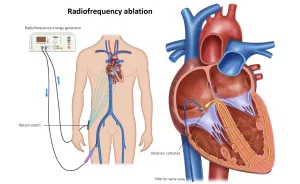
- Which surgery you had, and how it went. (Small repairs vs. big reroutes like a bypass.)
- Complications. Let’s hope for none, but if you do get an infection or have some rhythm hiccups, tack on extra weeks.
There are also financial questions no one loves to talk about, but… they matter. Planning for the Open heart surgery cost upfront saves you surprise stress mid-recovery.
The Two-Stage Recovery Dance
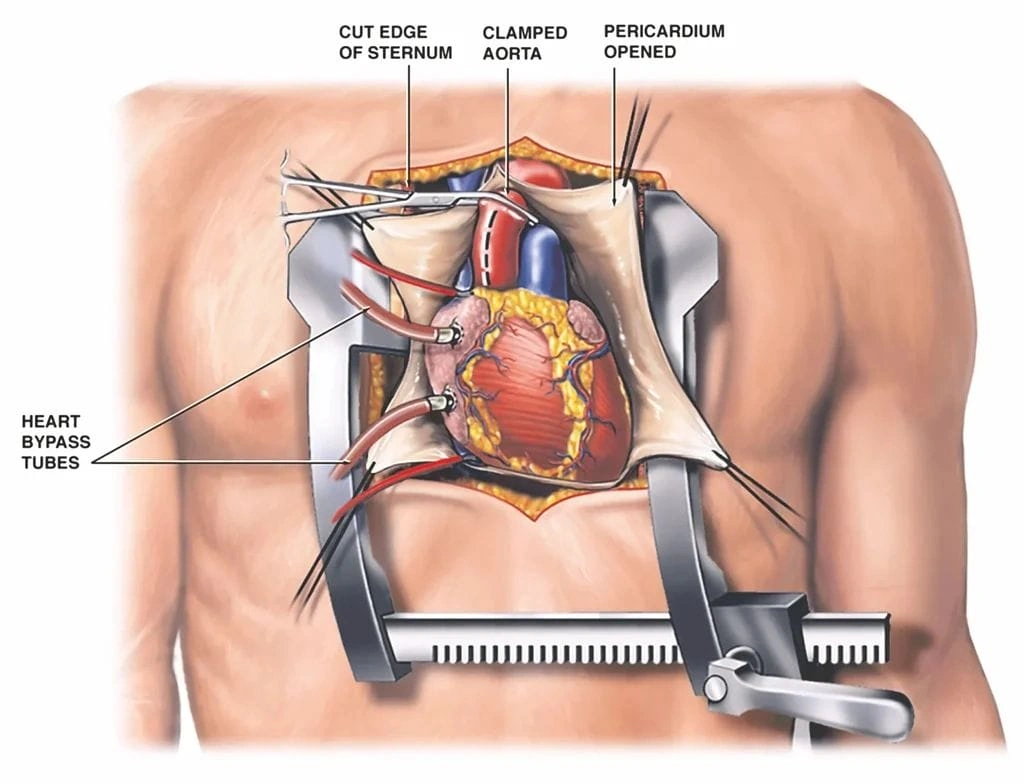
Stage one: hospital life. You’ll probably spend 5-ish days there (according to NGHS), starting in the ICU surrounded by machines, tubes, and nurses who somehow appear right when you think, “Hmm, is this normal?” Then you switch to a less intense room, maybe even a window view. It’s all about managing pain, learning breathing tricks, and honestly, feeling like a baby deer getting back on your feet.
Stage two: home sweet—wait, am I ready?—home. Here’s where time slows down and real questions kick in. “Can I walk to the bathroom? Is it weird that I’m so tired? When will food taste normal again?” All valid. Most recovery actually happens here, away from beeping machines, but with its own bumps.
Gritty Details: What Actually Happens Week by Week
The First 2 Weeks: The Slow Crawl
These days feel slow, and honestly, a bit achy (body and mood). Swelling? Yep, pretty normal for your legs—especially if you had bypass, since they borrow veins from there. Appetite? Meh, don’t push it. As for sleep, let’s just say it’s overrated for now. Those early days you might hear/feel some odd chest “clicks”—happened to my uncle and it freaked him out, but it’s normal, and usually fades by week two (Cleveland Clinic).
A lot of folks start feeling frustration here. My best friend’s mom said every shower felt like a marathon. Some days she celebrated getting dressed—other days, just sitting in the sun was a win. Go easy on yourself. Each victory matters.
Weeks 3 to 4: Life Gets Color Again
You’re moving more now. Walking, maybe circling your block, or puttering around the kitchen. (Don’t lift that cast-iron skillet yet!) Your surgeon should clear you for driving—usually by end of week four if all is well.
Pro tip: ask for milestones, not just time frames. For example, my ex-boss texted me, “Today I walked half a mile without needing to sit. Felt like Rocky!” His secret? Pacing himself and not making every day a test.
You might start getting hungry again, and (hooray!) taste buds often wake up. If you’re wondering about returning to your office desk, a lot of people get the green light around week 4 to 6. If you do physical work, plan for longer.
Weeks 5 to 8: Stronger by the Day
Here’s where you get into a groove. Daily life feels less like swimming through molasses. You can probably handle household chores (the light kind—don’t climb ladders or carry groceries that make your incision wince). By week 6, returning to sedentary office work is often okay, but always check with your doc.
At this stage, some people get a little cocky—hey, feeling good! Just remember, heavy lifting is still a no-no. I remember my neighbor, a stubborn guy in his 70s, tried to shovel snow at week seven. Didn’t end well… so, please don’t be him.
Weeks 9 to 12: Almost There (But… Pace Yourself!)
Many can return to normal routines—minus heavy gym sessions or super long trips. Cardiac rehab, if you haven’t started yet, becomes your new sidekick. It’s actually pretty fun, like guided fitness built for people who get you. According to this Henry Ford Health post, regular rehab helps you get back to “your normal” faster, and with better heart health long-term.
And yes—by now, you’re probably itching to be fully independent. Take advantage of follow-ups, and just peek at those stats on open heart surgery survival rate by age. They’ll show you how much this investment in yourself is worth it.
A Handy Table: Sample “Feeling Like Me Again” Timeline
| Week | What You’re Doing | Advice From Real Folks |
|---|---|---|
| 1 | Walking short hallway laps, naps galore, pain meds | Track small wins—and naps are productive! |
| 2 | Getting to the mailbox, prepping simple snacks | Ask for help… and don’t rush showering solo |
| 4 | Cleared to drive, doing bigger walks | Plan outings around where you can sit if tired |
| 6 | Back to (desk) work, maybe light chores | Stamina’s back—take it for a test drive, gently |
| 12 | Nearly “baseline”, might try group fitness or travel | Take rehab lessons with you for the long run |
That Weird Mix: Pain, Mood, and Those “Normal” Questions
Wait, Should I Still Hurt?
Let’s be honest—”normal” is a moving target in open heart surgery recovery time. Chest and shoulder aches stick around for weeks; sneezing can bring new respect for your ribcage. The good news? Pain usually fades steadily, but ask your team if you’re ever in doubt.
Mood swings or the blues creep in too. Turns out, it’s not just you. A lot of people feel flat, frustrated, or oddly emotional. (Seriously, my uncle wept at a puppy food commercial. Post-op hormones are wild.) Don’t hide it. Mention it to your doc—it’s super common and usually temporary.
Food, Sleep, and All the Rest: What’s Normal?
Food… honestly, it might taste weird for a stretch. Give those taste buds grace. Trouble sleeping is common, too—pain, new meds, or just the weirdness of hospital rhythms. Try a short walk every day and talk about med timing; both help.
Let friends and family pitch in. You’d be shocked how many people want to help—but need marching orders (“bring me soup, text me at noon, please vacuum!”).
A Real Talk on Money & Odds
Before I forget—Open heart surgery cost is never fun to face, but sorting finances ahead of time can really lower stress after surgery. A little planning means fewer “Oh, no!” moments when the bills land and you’re still tired from walking up the stairs.
And about those numbers: If you’re curious, open heart surgery survival rate by age is a surprisingly optimistic read for most age groups. Bottom line? Odds are on your side—especially if you stick with your doc and the rehab team.
Life After: Building Back Stronger
When Can I…?
Ready for some of the most-asked questions?
- Drive: Most can again after 4 weeks (when not taking strong meds).
- Return to work: Desk jobs are usually okay at 4-6 weeks. Heavy-duty jobs? 8-12 weeks or more. Play it safe.
- Lift things (kids, pets, etc.): “Nothing heavier than a gallon of milk for at least 6 weeks,” my friend’s surgeon joked—and she wasn’t kidding.
- Travel: Wait until you’re stamina-strong. If you must fly, clear it with your team.
Rehab: Your Secret Weapon
You know how athletes bounce back from injuries with a whole team behind them? Cardiac rehab is your team. It’s gentle training, nutrition talks, and a peer group that gets the awkward “tired halfway up the stairs” feeling. People who do rehab heal faster, feel more confident, and rebuild stamina in a safe way (research on Cleveland Clinic). Don’t skip it. Seriously.
Red Flags: When to Call the Doc
Don’t tough out real warning signs. These call for a quick call or visit: fever over 100°F, chest pain not fading, swelling that gets worse, sudden breathlessness, or anything that just feels “wrong.” Trust your gut. My ex-boss put off his call and landed back in the ER. You have permission to be “that” patient.
Wrapping Up: You’ve Got This (For Real)
Whew, that was a lot. If your head’s spinning, remember: you’re not alone. Open heart surgery recovery time is an up-and-down ride, but almost everyone gets their groove back—6, 8, 12 weeks, sometimes more. Give yourself permission to rest. Celebrate every little milestone, not just the big “all clear.”
Check in on open heart surgery cost early, so it’s one less surprise. And if you need a confidence boost, skim those open heart surgery survival rate by age stats—recovery really is worth it.
Your next step: Go easy, make that follow-up appointment, nap proudly, and—this is crucial—track your small wins. And hey, if you’re feeling uncertain, frustrated, or just want to swap “zipped-up” stories, reach out. Someone (maybe me!) will cheer you on. This is your comeback story, one slow, weird, and wonderful step at a time.

















Leave a Reply
You must be logged in to post a comment.